Your Scan Says "Hepatic Steatosis" But Your Doctor... | Gut Check Daily

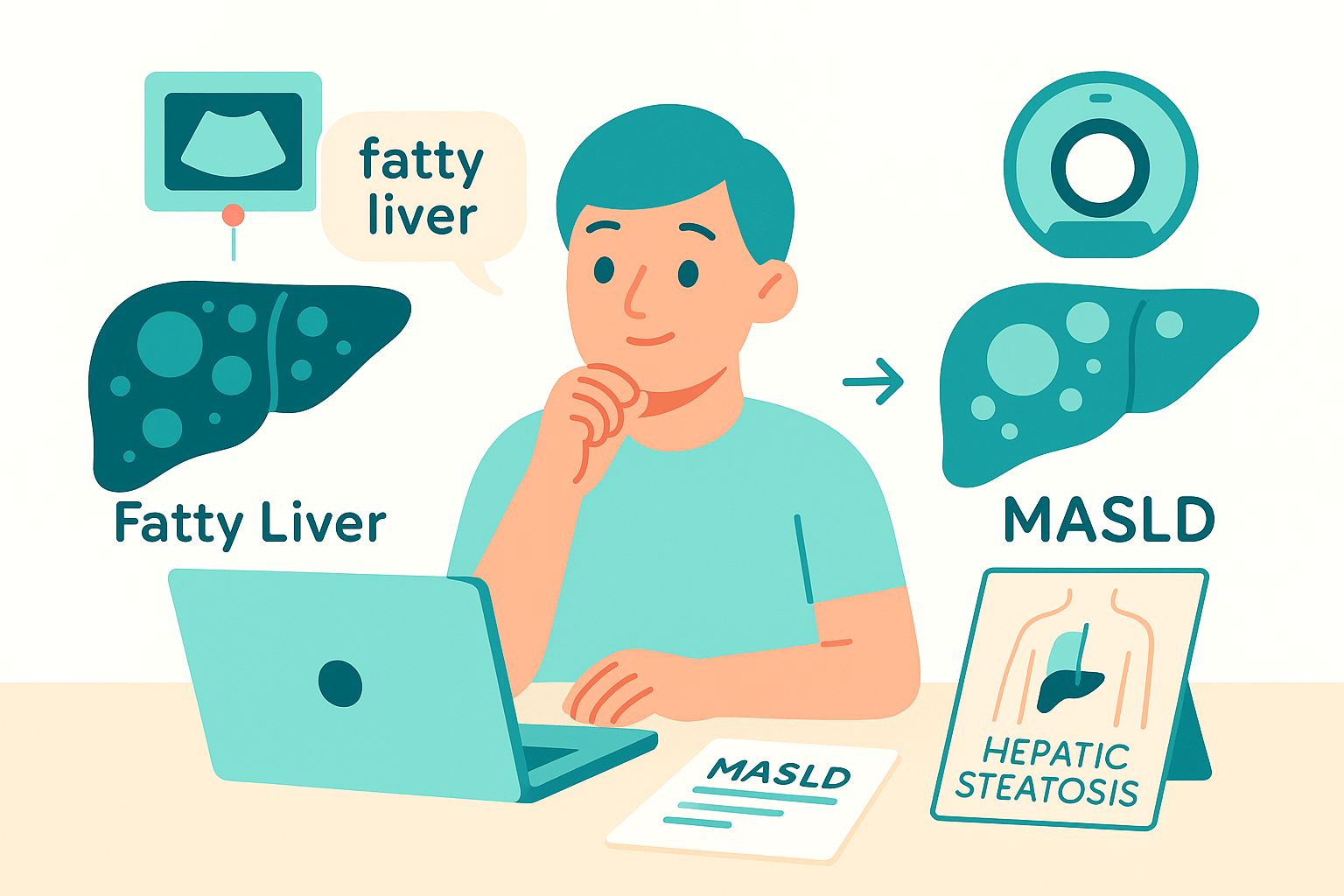
So you got an ultrasound or CT scan for something totally unrelated, and boom – the radiologist mentions "hepatic steatosis" (fancy medical term for fat in your liver). Now you're Googling at 2am wondering if you're dying. Let me break this down the way I wish more docs explained it to patients.
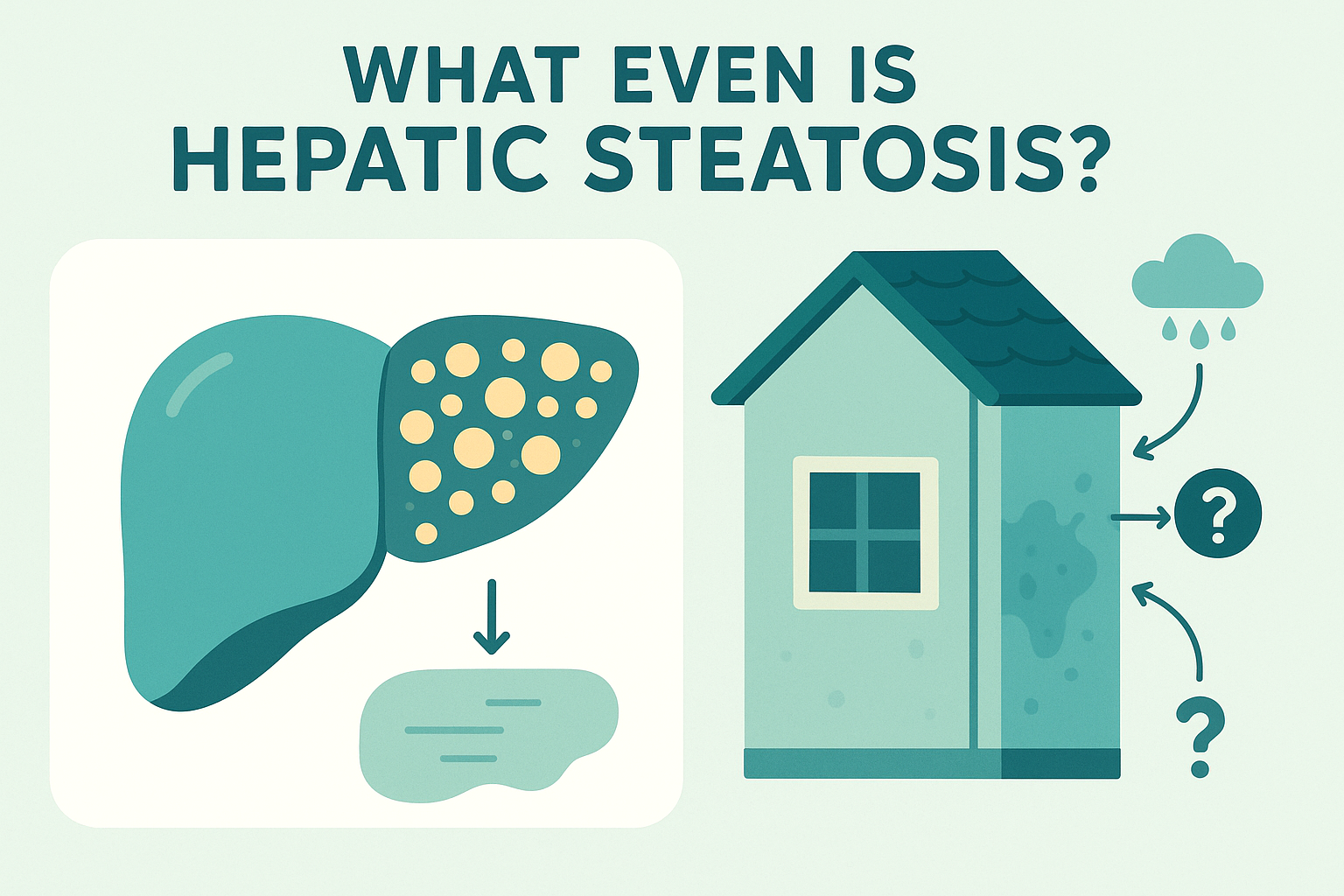
First: What Even Is Hepatic Steatosis?
Hepatic steatosis just means fat is hanging out in your liver cells where it shouldn't be. Think of it like finding water damage in your house - you know there's a problem, but you don't know WHY yet. Could be a leaky pipe, could be a roof issue, could be condensation. The water stain is the finding; now we need to figure out what caused it. Same deal with fatty liver. The imaging shows fat accumulation, but that's not a diagnosis, it's a finding that makes us ask "okay, what's causing this?" The Usual Suspects We Check For: When we see fat in your liver, we run through a whole checklist of potential causes:
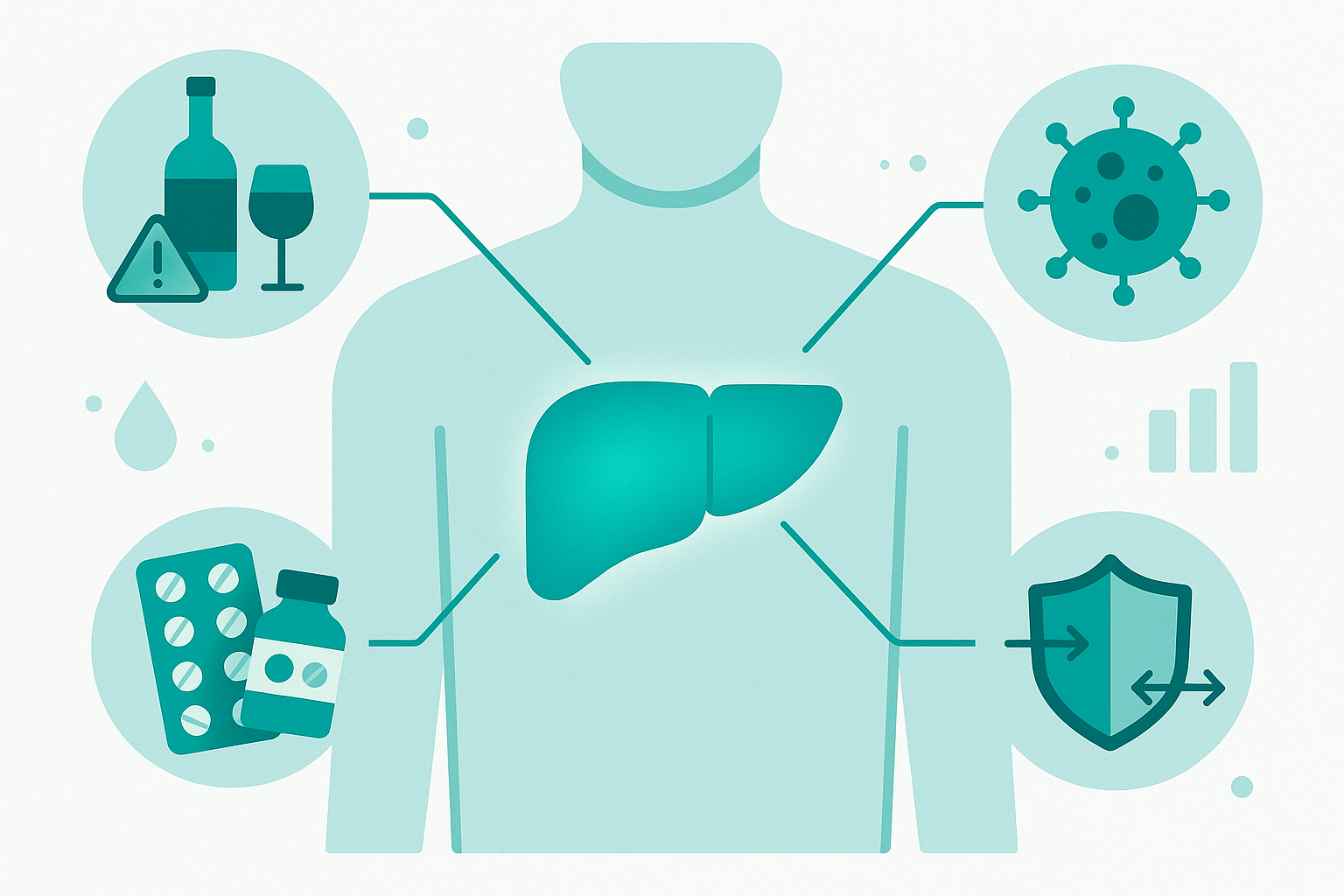
Metabolic issues: insulin resistance, diabetes, obesity, high triglycerides, high blood pressure (this is MASLD, formerly called NAFLD)
Alcohol: and we're talking more than you might think qualifies as "significant". Medications: steroids, certain chemo drugs, methotrexate, amiodarone, tamoxifen, and others. Viral hepatitis: Hep C especially can cause steatosis. Autoimmune hepatitis: your immune system getting confused and attacking your liver. Wilson's disease, hemochromatosis – genetic disorders affecting copper or iron Celiac disease. Also rapid weight loss or malnutrition, counterintuitively, this can also cause fatty liver Other rarer stuff like TPN (IV nutrition), certain genetic lipid disorders, etc.
We sort through this with blood work (liver enzymes, metabolic panel, hepatitis serologies, autoimmune markers, iron studies, etc.) and your clinical history (do you drink? What meds are you on? Family history?).
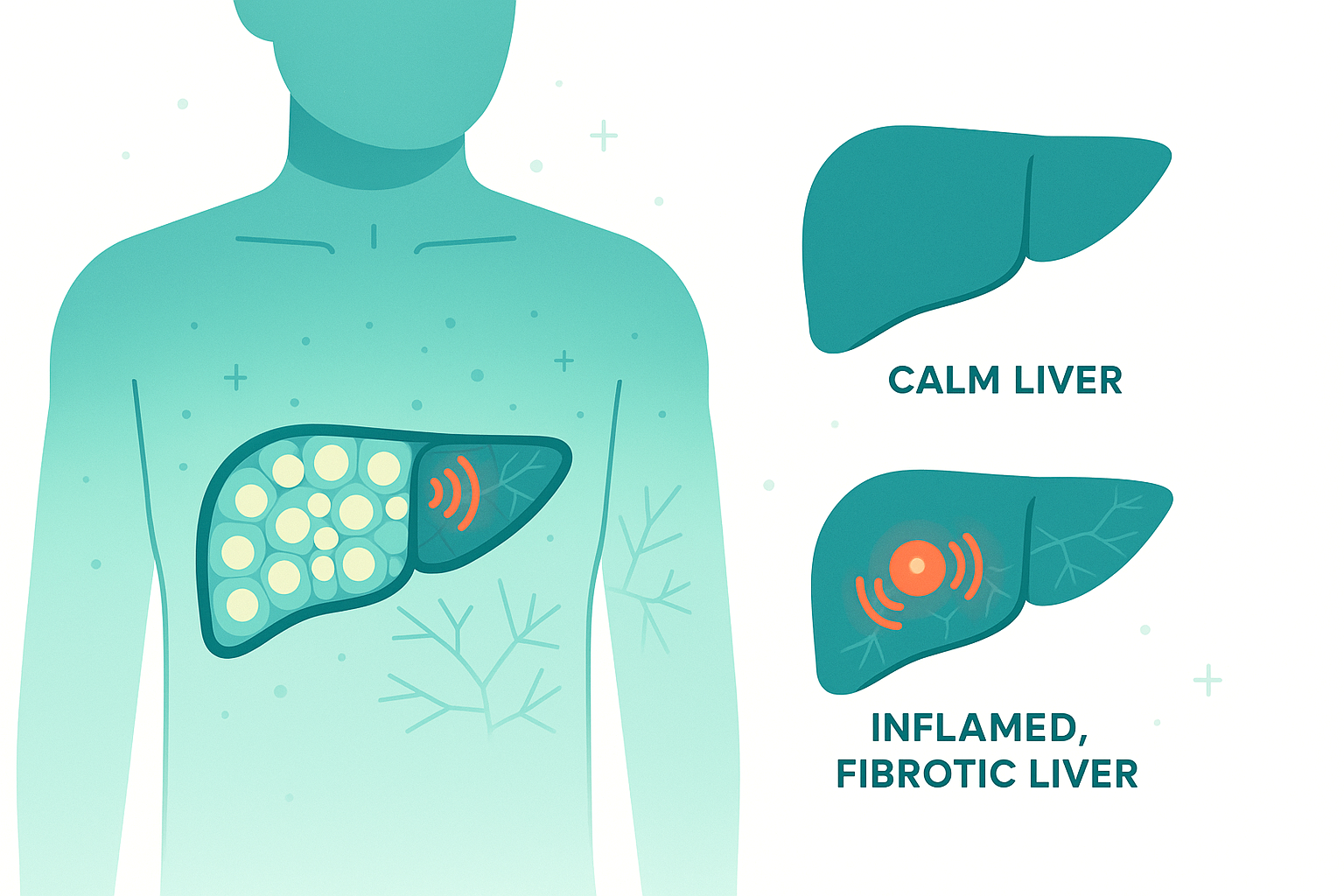
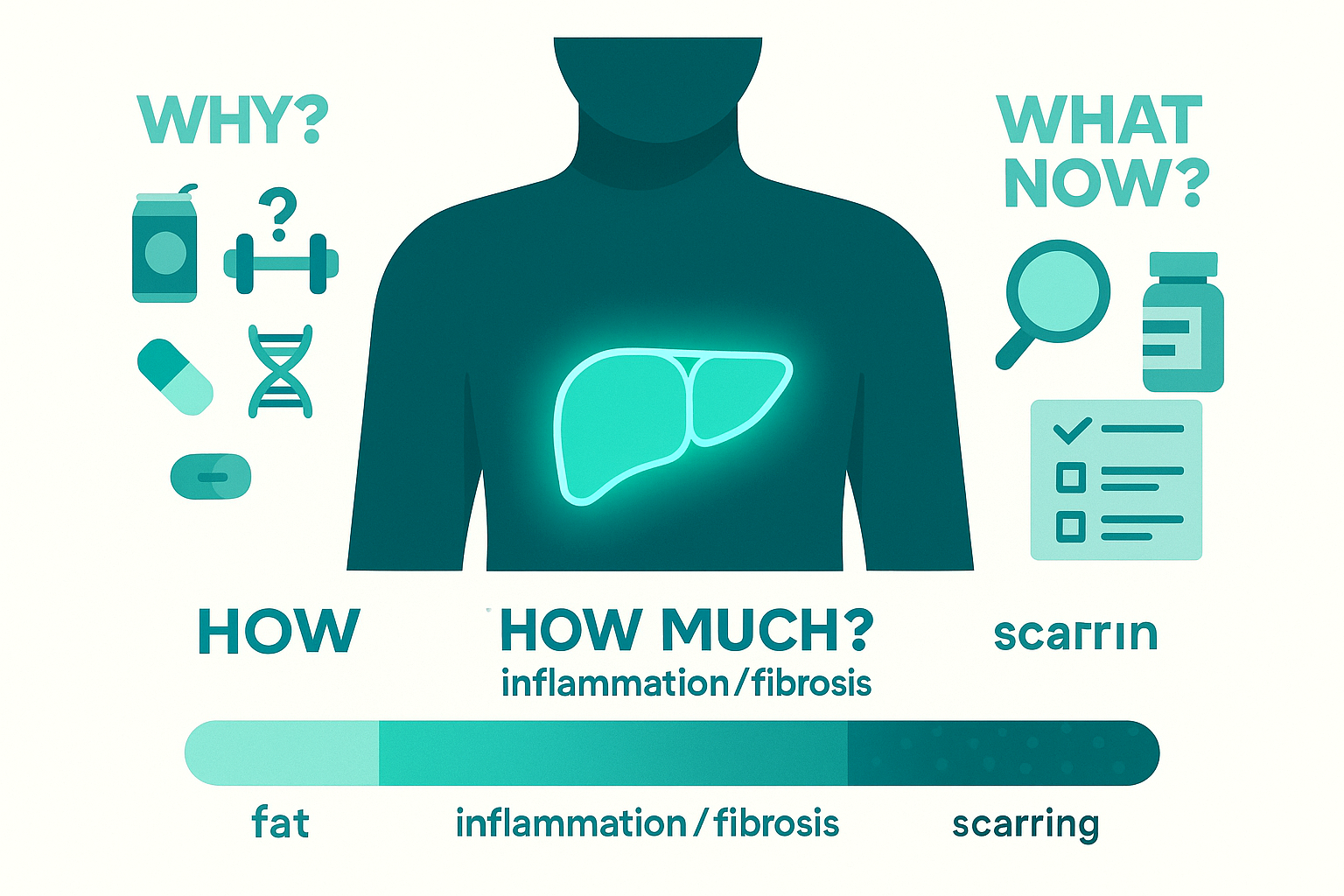
Why Do We Even Care About Fat in the Liver?
Here's the part that matters: fat is metabolically active and pro-inflammatory. It's not just sitting there inert like packing peanuts. Those fat droplets in your liver cells trigger inflammation. Over time, chronic inflammation leads to fibrosis (scarring). If that fibrosis keeps progressing, you eventually get cirrhosis (extensive scarring that disrupts liver architecture and function). And cirrhosis brings a whole mess of problems: portal hypertension, liver failure, increased cancer risk, etc. The progression looks like:
Simple steatosis (just fat, minimal inflammation) Steatohepatitis (fat + inflammation) - this is where "MASH" comes in Fibrosis (scarring starts) Cirrhosis (extensive scarring, permanent damage)
Not everyone progresses through all these stages, but we can't predict who will, so we take it seriously.
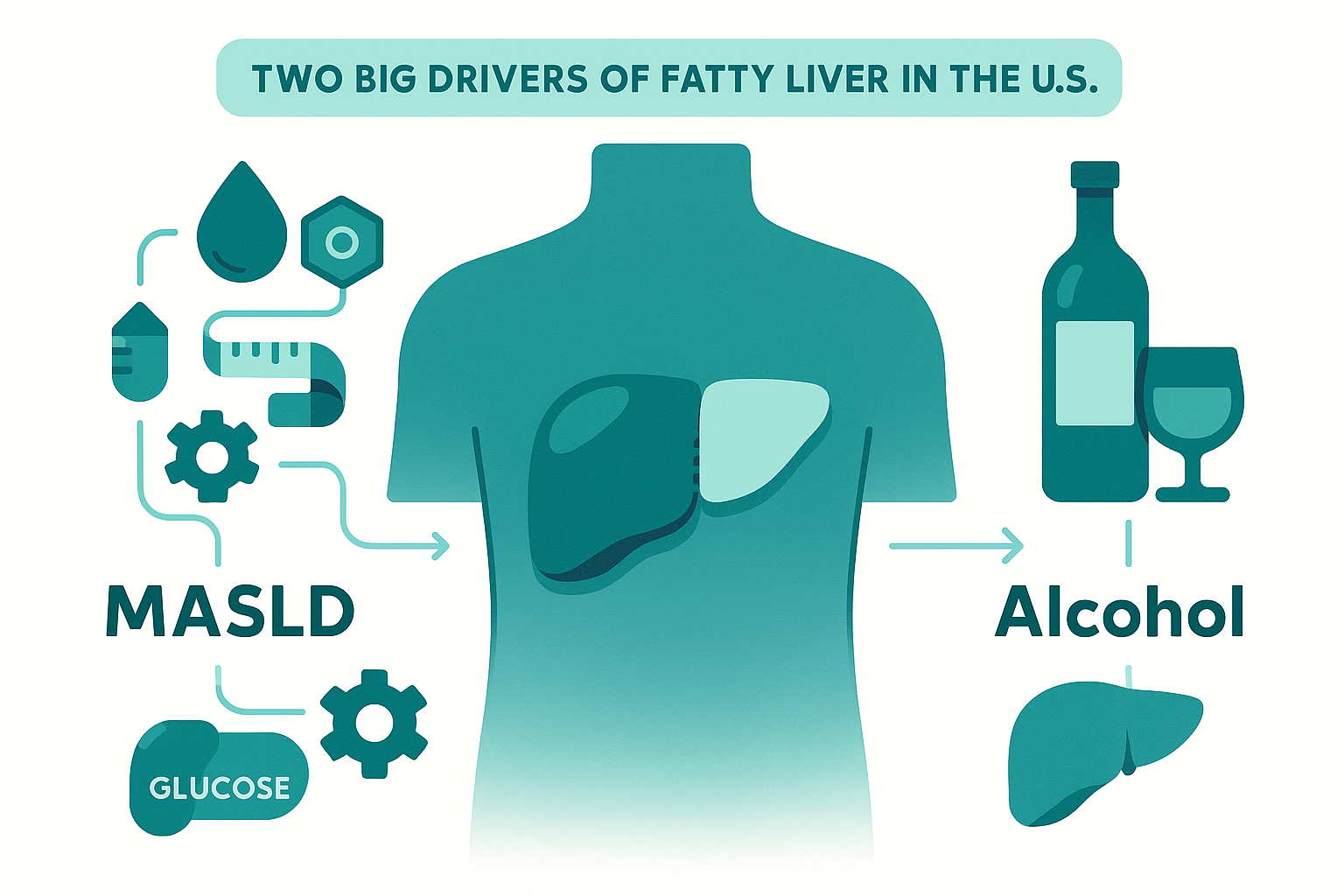
MASLD vs Alcohol: The Two Big Players in the US
In the United States, metabolic dysfunction and alcohol are far and away the two most common causes of fatty liver. MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease) is the new name for what we used to call NAFLD (Non-Alcoholic Fatty Liver Disease). The name change reflects better understanding – it's not just about not drinking; it's about metabolic dysfunction driving the process. We're talking insulin resistance, visceral obesity, dyslipidemia, hypertension – the whole metabolic syndrome package. Alcohol-related liver disease is exactly what it sounds like. The tricky part is defining "significant" alcohol use – for women, we're generally talking >7 drinks/week or >3 drinks per occasion; for men, >14 drinks/week or >4 per occasion. But there's huge individual variation in susceptibility. Sometimes people have BOTH going on, which is now called MetALD (Metabolic and Alcohol-related Liver Disease). Your liver doesn't care about our neat diagnostic categories.
Do You Need a Liver Biopsy?
Usually not. Liver biopsy used to be the gold standard for staging disease, but it's invasive, expensive, has risks (bleeding, infection, pain), and suffers from sampling error (we're only looking at a tiny piece of a large organ). We typically reserve biopsy for situations where:
Non-invasive testing gives conflicting results We suspect multiple causes happening simultaneously We need to rule out other diagnoses (like autoimmune hepatitis) Imaging or labs suggest advanced fibrosis but non-invasive scores are discordant Clinical trial enrollment requires histologic confirmation
So How DO We Monitor It?
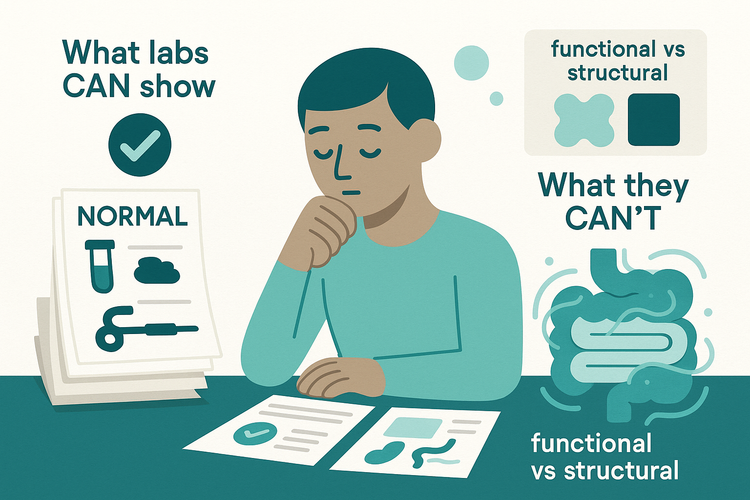
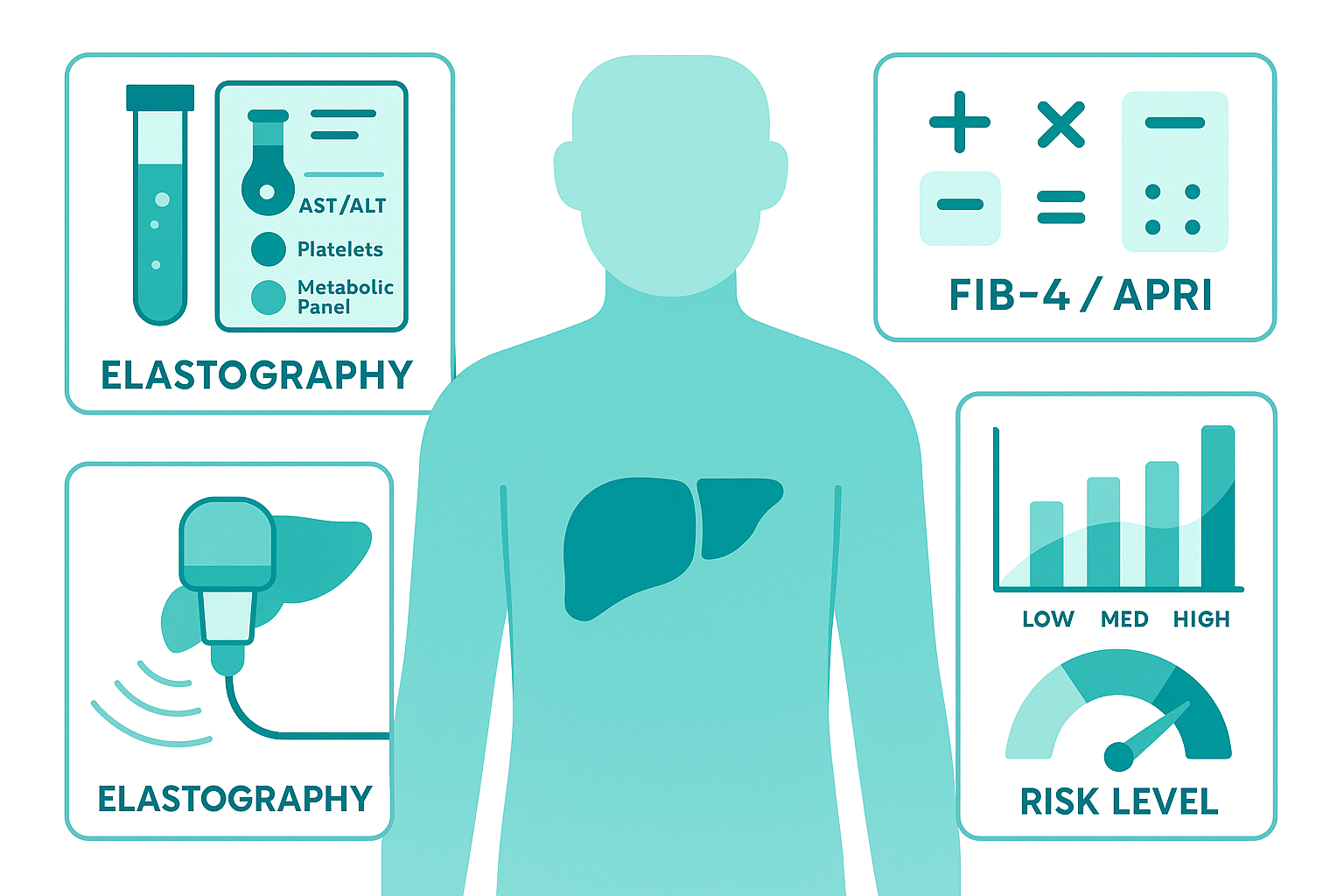
Blood work:
Liver enzymes (AST, ALT) – though these can be totally normal even with significant disease Platelet count – drops as fibrosis advances Metabolic panel – glucose, lipids, kidney function Calculated scores like FIB-4 or APRI that use lab values to estimate fibrosis risk
Elastography (FibroScan or MR elastography): This is the game-changer. Non-invasive, quick, and gives us a stiffness measurement that correlates with fibrosis stage. Not perfect, but way better than biopsying everyone. We can track this over time to see if things are improving, stable, or progressing. Some centers also use specialized MRI techniques (MRI-PDFF) to quantify fat percentage in the liver.
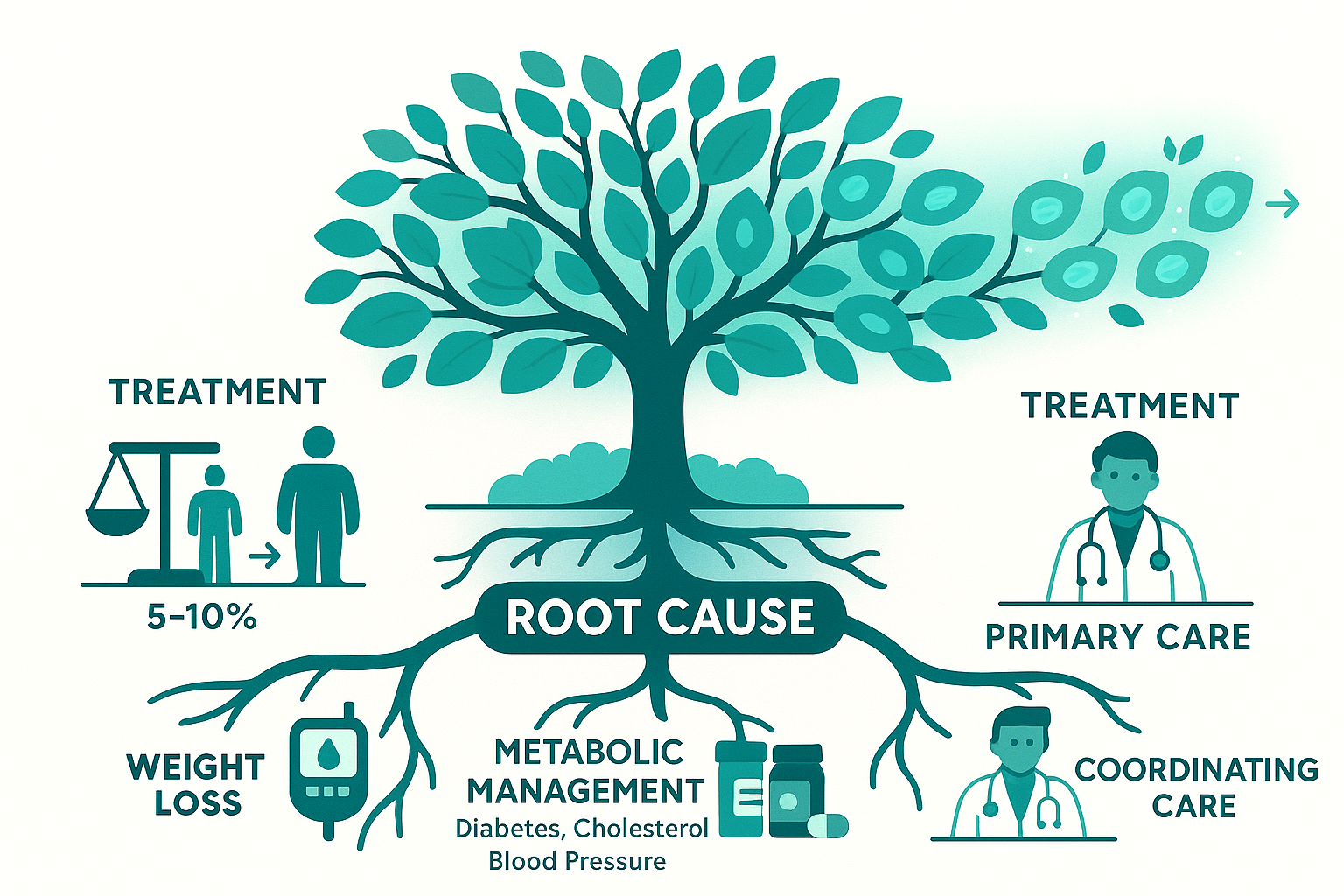
Treatment: It's Mostly About the Root Cause
Here's where the rubber meets the road: For MASLD:
Weight loss, even 5-10% body weight reduction can significantly improve liver fat and inflammation. This is the foundation. Metabolic management, usually coordinated by your PCP: controlling diabetes, managing cholesterol, treating hypertension. Exercise, independent benefit beyond just weight loss. Diet, Mediterranean diet has good evidence; avoid excessive fructose and processed foods. GLP-1 agonists, BIG development here. Drugs like semaglutide (Ozempic/Wegovy) and tirzepatide (Mounjaro/Zepbound) are showing impressive results. In 2024, resmetirom became the first FDA-approved medication specifically for MASH with fibrosis. This is a huge deal because we finally have targeted pharmacotherapy.
For alcohol-related liver disease:
Complete alcohol cessation is what matters. Addiction medicine support if needed (naltrexone, acamprosate, behavioral therapy) Nutritional support (thiamine, folate, often malnourished)
For other causes:
Stop the offending medication Treat the underlying condition (hepatitis, autoimmune disease, etc.)
The Bottom Line
"Fatty liver" is super common, probably around 25-30% of US adults have it. Most people with simple steatosis won't progress to cirrhosis, but some will, and we can't perfectly predict who. The important thing is:
Figure out WHY you have fat in your liver (hence the workup) Assess how much inflammation and scarring is present (blood work, elastography) Address the underlying cause (metabolic management, stop drinking, etc.) Monitor over time to make sure things aren't progressing
It's not an emergency, but it's not something to ignore either. Work with your doctor (usually your PCP, sometimes a hepatologist if things are more advanced) to address the root cause. And hey, if you're reading this at 2am after getting your ultrasound results - take a breath. You're going to be okay. Make an appointment with your doctor, get the appropriate workup, and go from there. Most people with fatty liver never progress to serious disease, especially if they address it early.