Remission in Ulcerative Colitis: Lessons From a Viral Reddit Thread

Remission In Ulcerative Colitis Lessons From A Viral Reddit Thread
Download this comprehensive checklist to bring to your next GI appointment. Get evidence-based answers and a clear action plan.
📥 Download PDF Checklist →
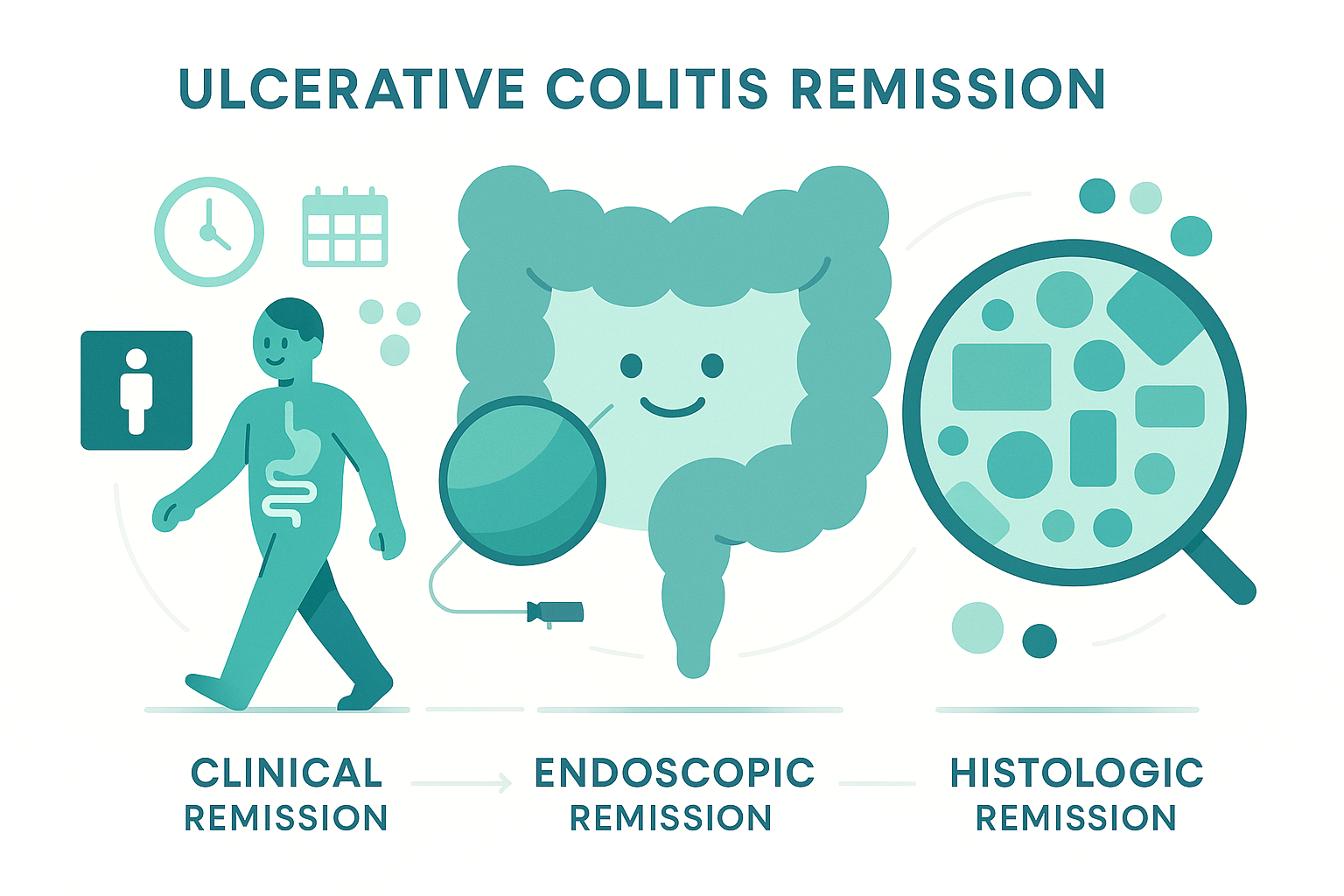
1. The three kinds of remission in UC
When doctors say “remission,” they’re often talking about one of three very different things:
1) Clinical remission
This is the one you feel.
Roughly means:
• No visible blood
• Near-normal bowel movements for you
• No urgent “I need a bathroom NOW or I’m in trouble” dashes
• You’re living your life without UC dominating your day
This is what most patients (reasonably) care about first. It’s also the main focus of older research and some older guidelines.
2) Endoscopic remission
This is what the camera sees on colonoscopy.
Typical definition in modern studies and guidelines:
• No ulcers
• No obvious friability or inflammation
• On common scoring systems (like the Mayo endoscopic subscore), this usually means 0 or sometimes 0–1
You can feel awful and still have a “pretty good” scope. You can also feel fine and still have mild inflammation.
3) Histologic remission
This is what the pathologist sees under the microscope.
Biopsies are taken even from areas that look normal. The pathologist is looking for things like:
• Neutrophils (a type of white blood cell) actively attacking the lining
• Ulceration or erosions at the microscopic level
• Architectural distortion from chronic damage
Histologic remission means those signs of active inflammation are gone. The tissue looks “quiet” at the cellular level.
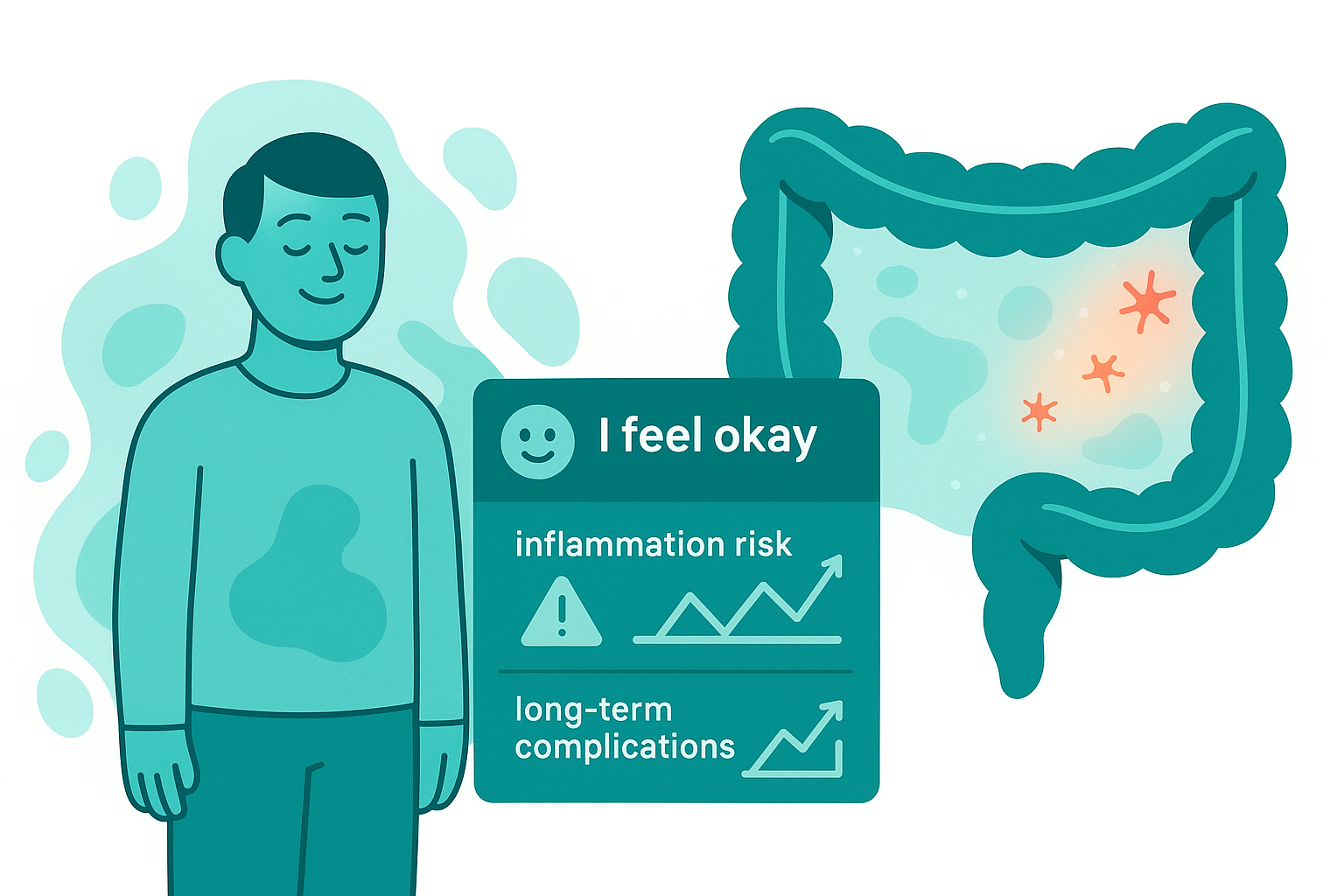
Why it matters: Multiple studies now show that patients who reach histologic remission have:
• Lower relapse rates
• Fewer hospitalizations
• Lower risk of colectomy
• Lower colorectal cancer risk over time
That doesn’t mean histologic remission is the only reasonable target for everyone, but it explains why your GI might still be pushing treatment even when you feel okay.
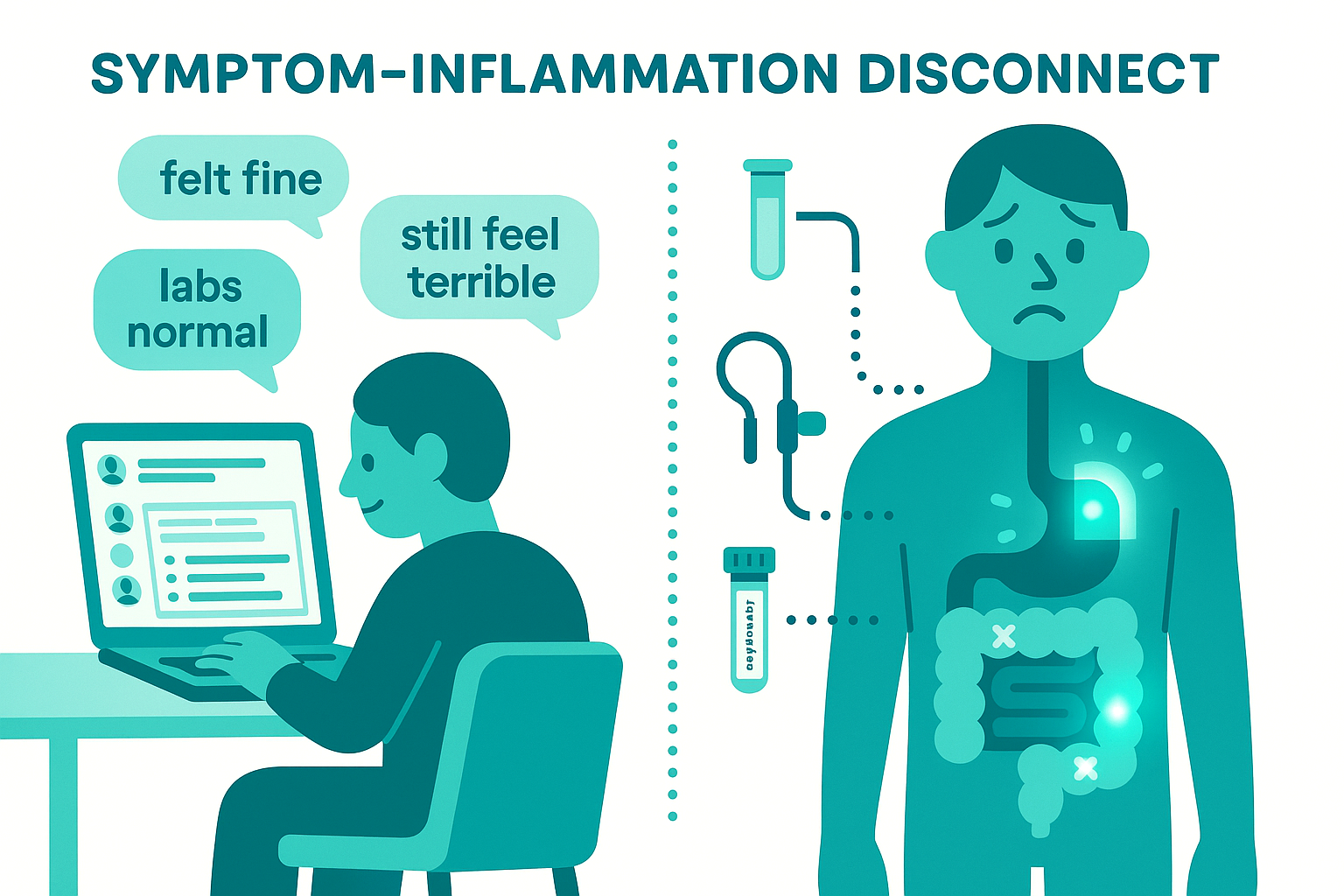
2. The symptom–inflammation disconnect: why your story matches that Reddit thread
From the comments on the post, you see the same patterns over and over:
• “I felt fine, but my scope showed inflammation everywhere.”
• “My biopsies were ‘quiescent’ but I still feel terrible.”
• “Calprotectin was normal, but I was clearly flaring.”
• “Scopes and labs are better, but my symptoms are worse.”
This disconnect shows up in several ways:
A. You feel good, but inflammation is still there
Examples from the thread:
• Clean-ish scope but biopsies show inflammation throughout
• Mild symptoms or no symptoms, but calprotectin 200–900
• “Quiet” inflammation on pathology, but you know something is off
Why this matters:
• Ongoing inflammation (even mild) means repeated cycles of injury and repair in the colon.
• Every cycle of repair carries a small chance of DNA error, which is how long-term inflammation increases cancer risk.
• People with persistent microscopic inflammation tend to relapse sooner than people in true histologic remission.
So from a long-term perspective, “I feel okay” plus “ongoing inflammation” is not the win it seems.
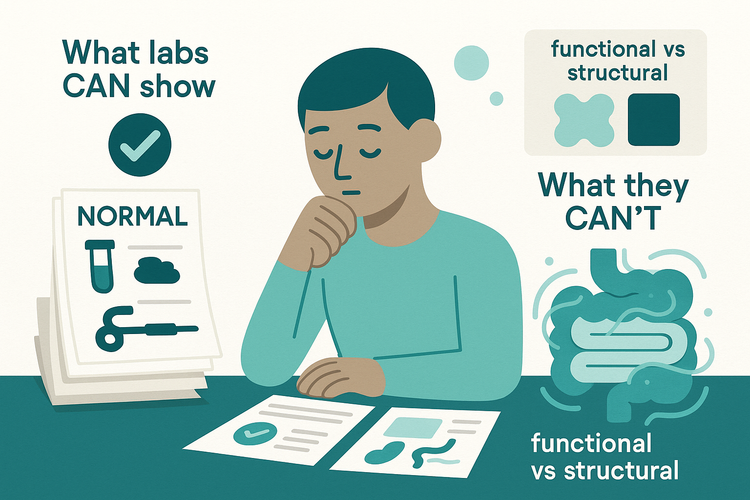
B. You feel awful, but tests look reassuring
Multiple people in the comments describe:
• Clean colonoscopy, low calprotectin, but diarrhea, urgency, pain
• Colonoscopy improved but symptoms worse right after prep
• “In remission” on paper, but daily suffering
Common explanations:
• IBS overlay (very common in people with IBD)
• Visceral hypersensitivity after years of inflammation
• Pelvic floor dysfunction
• Side effects from meds, infections, SIBO, or something non-IBD
In these situations, treating inflammation harder doesn’t always help because the inflammation may already be under control. You need different tools (diet tweaks, gut–brain modulators, pelvic PT, etc.) rather than more immunosuppression.
Bottom line: symptoms are real and important, but they are not a perfect thermometer for inflammation.

3. How we actually measure inflammation (and what can go wrong)
Most of the questions in the thread were really about this: “How do I know what’s actually going on in my colon without being scoped constantly?”
Here are the main tools and their tradeoffs.
A. Fecal calprotectin
What it is: A protein released by neutrophils in the gut that shows up in stool. Higher calprotectin usually means more intestinal inflammation.
Why we like it:
• Non-invasive
• Correlates better with mucosal inflammation than blood markers or symptom scores in many studies
• Very useful for tracking trends over time
• Helps decide when a scope is needed
Why it’s imperfect:
• Some people’s calprotectin does not track their disease well (a few in the thread mention this)
• Upper GI inflammation, infections, NSAID use, and other issues can also raise it • Cut-off values are not one-size-fits-all; a “borderline” number might be very meaningful in one person and noise in another
Practical use case:
• Most useful when you’ve had several calprotectin tests paired with scopes/biopsies, so you and your GI know how your body behaves.
• Once that pattern is known, calprotectin can often be used between scopes to monitor disease and dose changes without scoping every time.
B. Blood tests
Common ones:
• CRP (C-reactive protein)
• ESR
• Hemoglobin, iron studies
• Platelets, WBC count, albumin, etc.
Pros:
• Simple, widely available
• Trends can support the story (rising CRP + symptoms + high calprotectin = inflammation is very likely)
Cons:
• Many people with UC, especially with disease limited to the rectum or left side, have normal CRP even in active disease.
• CRP and ESR can be elevated from infections, obesity, other inflammatory conditions, etc.
Blood tests are supporting actors, not the main character.
C. Colonoscopy + biopsies
Pros:
• Gold standard for directly visualizing inflammation
• Allows scoring of disease activity and distribution
• Biopsies provide histologic grading and dysplasia surveillance
Cons raised in the thread:
• Cost and access (very real in the US)
• Anxiety, logistical burden
• Some people experience post-scope flares or feel worse after prep
• Pediatric patients often have fewer surveillance scopes and rely more on biomarkers and symptoms
Even with those caveats, colonoscopy with biopsies remains the backbone for:
• Confirming diagnosis
• Assessing true disease severity
• Deciding on major treatment steps (biologic start/switch, confirming deep remission, cancer surveillance)

4. What “treat to target” means in real life
Over the last decade, inflammatory bowel disease care has moved toward a “treat to target” approach, summarized by STRIDE and STRIDE-II guidelines.
Core idea:
• Instead of “treat until you feel better, then hope for the best,” we:
• Define clear targets (clinical remission, endoscopic healing, and increasingly histologic healing)
• Monitor those targets with objective tests
• Adjust treatment when we’re off target, even if symptoms seem “okay”
STRIDE-II highlights:
• Short-term: symptom relief, improved quality of life
• Medium-term: normalization of biomarkers like CRP and calprotectin
• Long-term: endoscopic healing; histologic healing is not yet a formal target but is recognized as a strong predictor of better outcomes.
What this looks like for you:
• When you start or escalate a med, the goal is not just “you feel better.” We also want proof that inflammation is under control.
• Once you’re stable, we can often increase the spacing between scopes and rely more on non-invasive markers that have proven reliable for you.
• Changing or escalating therapy should be a shared decision, not a unilateral decree. That includes weighing:
• Your symptom burden
• Your risk tolerance
• Cancer risk factors
• How much residual inflammation is present
• Access, cost, side effect profile
There is also emerging debate and nuance: not every study shows extra benefit from pushing all the way to complete histologic normalization in everyone, especially once endoscopic healing is achieved. So “ideal textbook target” and “real-world appropriate target for you” may not always be identical.
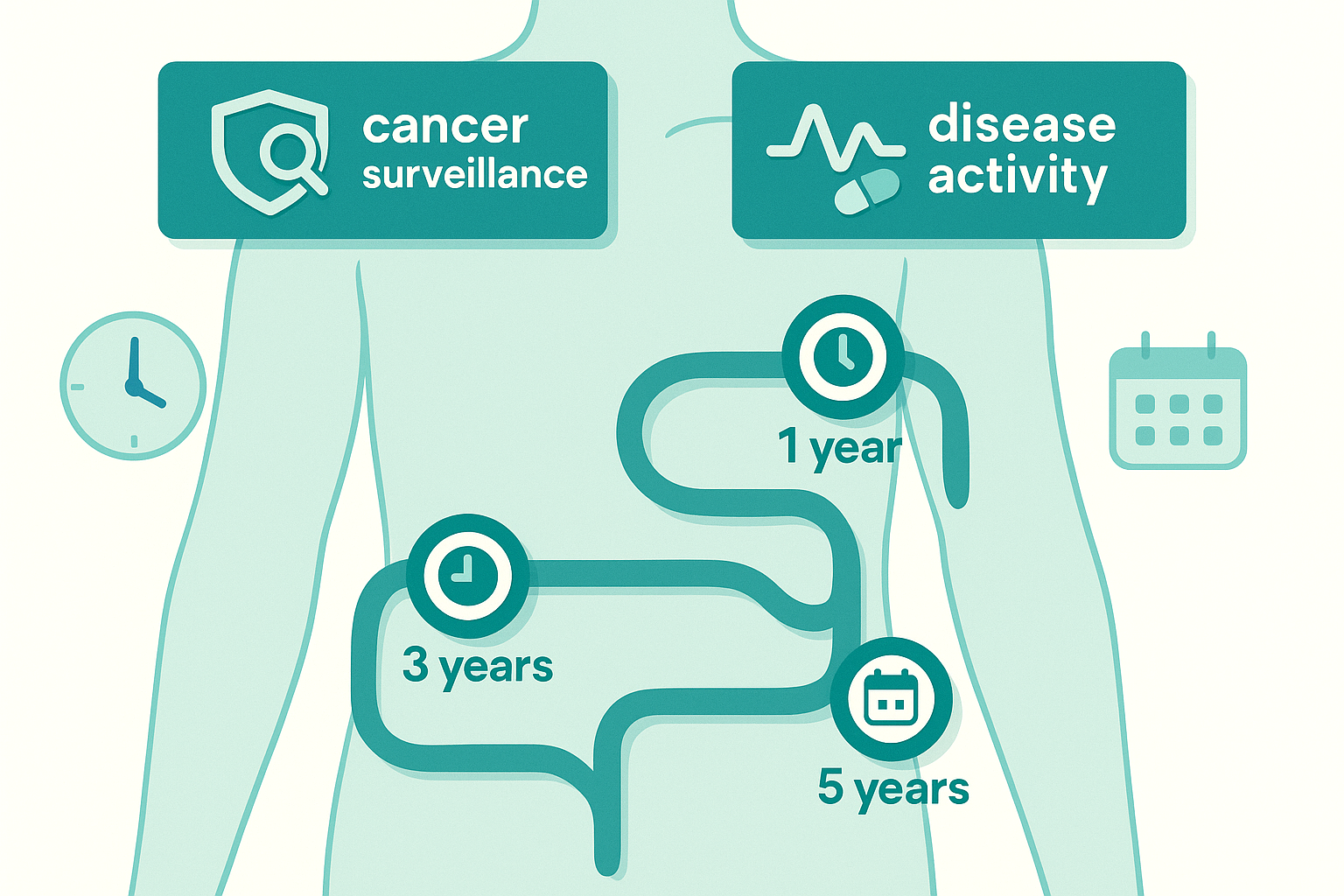
5. How often should you have colonoscopies?
This came up repeatedly in the comments: “My GI said 5 years,” “Mine said yearly,” “Is three years too long?”
There are two separate questions: 1. Cancer surveillance 2. Assessing disease activity / treatment response
1) Cancer surveillance
Most major societies agree on roughly:
• Start surveillance around 8 years after colitis onset (for disease that extends beyond the rectum).
• Repeat every 1–3 years depending on:
• How much of the colon is involved
• How long you’ve had disease
• How much chronic inflammation you’ve had
• Presence of PSC (primary sclerosing cholangitis)
• Family history of colorectal cancer
• Any prior dysplasia or polyps
This is about cancer risk, not flare control.
2) Assessing disease activity
Scopes may be done:
• To confirm how severe a flare really is
• To check if a new medication has actually healed the colon
• When symptoms, labs, and calprotectin disagree
• When diagnosis is uncertain or complications are suspected
Intervals here vary widely:
• Soon after starting a biologic or small molecule, some clinicians will re-scope within 6–18 months to see if you’ve hit endoscopic or histologic remission.
• If you’re stable clinically and with biomarkers that match prior scope findings, your GI may space scopes further apart.
There is no one right answer for everyone. A 25-year-old with pancolitis, PSC, and frequent flares is not going to have the same strategy as a 60-year-old with mild left-sided disease and long-standing deep remission.
6. When data and symptoms don’t match: two common scenarios
Scenario A: “I feel fine, but my colon looks angry.”
This was one of the most common and emotionally loaded situations in the comments.
Why GIs often push harder here:
• Persistent inflammation is what drives complications over the long arc: strictures, hospitalizations, surgeries, and cancer
• Waiting until you feel sick again often means you’re already behind.
What a reasonable plan might include:
• Confirming the findings: reviewing endoscopy images, pathology report, and calprotectin trends together
• Discussing options: optimizing current med (dose, route, adding rectal therapy), switching classes, or adding a biologic / small molecule
• Talking openly about your fear of changing something that “seems to be working” and balancing that against the long-term risk of quietly smoldering disease
• Negotiating a middle path: for example, modest escalation plus closer biomarker monitoring, with a clear plan for re-scoping.
Scenario B: “My reports say remission, but I feel terrible.”
Also very common in the thread.
This is where you want your team to:
• Double-check: • Any small areas of mild inflammation that were downplayed?
• Any missed infections (C. diff, CMV, parasites, etc.)?
• Bile acid diarrhea, SIBO, celiac, pancreatic issues?
• Look outside classic UC:
• IBS overlay
• Pelvic floor dysfunction
• Extraintestinal pain syndromes
• Medication side effects
• Non-GI conditions (thyroid, anemia, etc.)
It is reasonable in this scenario to:
• Ask for your full colonoscopy and pathology reports, not just “it was fine.”
• Ask: “If inflammation truly looks quiet, what’s our working diagnosis for my ongoing symptoms, and how are we treating that?”
Your symptoms are not “invalid” just because the colon looks clean. They may just need a different toolkit.

7. Practical questions from the thread, answered in plain language
“Should I push for more scopes if I’m feeling good?”
Maybe, but not blindly.
Good reasons to discuss an earlier scope:
• You’ve never had a “post-treatment” scope to confirm healing after starting a biologic or new regimen.
• Calprotectin or blood markers are trending up despite good symptoms.
• You had significant inflammation on your last scope and are now on a stable med plan; confirming histologic remission at least once can shape future monitoring.
Reasonable to wait:
• If you recently had a high-quality scope with good prep and biopsies
• You’re in stable clinical remission, and your biomarkers have historically tracked well
• You’re already on a maximized regimen with no realistic next step, and your GI thinks the result would not change management.
“How often should I check calprotectin?”
Depends on where you are in the journey:
• Early / changing meds: every few months can help track response
• Stable deep remission with known correlation to scopes: maybe every 6–12 months, or when symptoms change
• If it has never correlated for you: it may be of limited use; no need to throw money at a test that doesn’t match your disease biology
“Do breakthrough flares on a biologic mean it’s failing?”
Not always.
Key questions:
• Was there an obvious trigger (infection, antibiotics, new med, missed dose)?
• How long did the flare last, and what did calprotectin do?
• What do biopsies show now?
Sometimes:
• A short-lived “blip” that settles with temporary steroids and still shows good endoscopic healing can be compatible with overall effective maintenance therapy.
• Repeated or prolonged flares, or rising calprotectin despite adequate drug levels, may point to loss of response and need for optimization or switch.
Drug levels and antibody tests (for drugs like infliximab or adalimumab) can help here.
“What about scopes triggering flares?”
Many people report feeling worse after prep or scope:
• The prep itself can disrupt the microbiome and irritate an already sensitive gut.
• Gas insufflation and scope trauma can temporarily worsen symptoms.
But if every scope is described as “totally clean” and you repeatedly flare badly afterward, it is reasonable to discuss:
• Whether the prep type can be changed
• Whether the frequency is truly necessary
• Whether other monitoring tools can safely replace some scopes in your specific case
This is exactly the kind of situation where treat-to-target has to be adapted to the person, not followed as a rigid algorithm.

8. A simple checklist to bring to your next GI visit
You don’t need to memorize STRIDE, histology scores, or endoscopic indices. You do need a framework.
Bring these questions:
1. “Which kind of remission am I in right now?”
• Clinical, endoscopic, histologic? Which ones are confirmed, which are assumed?
2. “What are my monitoring tools?”
• Do my calprotectin values track with my colon?
• How often should we repeat labs, calprotectin, and scopes if I stay stable?
3. “What is our long-term target?”
• Are we aiming for endoscopic remission? Histologic remission? Why or why not for me?
4. “How will today’s decision change my 10–20 year outlook?”
• Not just next week’s symptoms.
5. “If data and symptoms don’t match again, what’s our next step?”
• Agree in advance how you’ll handle “I feel bad but tests look good” or the reverse.
6. “Can I get copies of my reports?”
• Colonoscopy report, pathology, calprotectin trends. Keeping your own file makes follow-up care much safer and more consistent.

9. The real goal: fewer surprises, more control
Ulcerative colitis will always involve some uncertainty. You can’t feel your calprotectin. You can’t see your rectum. You can’t predict every flare.
But you can:
• Understand the difference between feeling well and being truly quiet at the tissue level
• Use that knowledge to have more specific, less frustrating conversations with your GI
• Push for shared decision making instead of being told “you’re fine” or “we’re escalating” without context
• Advocate for appropriate cancer surveillance without over- or under-scoping
“Feeling good” matters. Your day-to-day life is the whole point of treatment. But for a disease measured in decades, how your colon is doing when you aren’t looking matters too.
Your job is not to become a pathologist or guideline expert. Your job is to bring your lived experience and your questions. The medical side is there to bring the tools and the data.
When those two pieces are used together, remission stops being a vague label and starts becoming a plan.