Implementing Low FODMAP for IBS Like A Pro

Low Fodmap Run It Like A Pro
Download this comprehensive checklist to bring to your next GI appointment. Get evidence-based answers and a clear action plan.
📥 Download PDF Checklist →The Low FODMAP diet gets thrown around like a magic fix, but most people are handed a random food list and zero strategy. Then you feel worse, more restricted, and terrified of apples. Let’s fix that. Low FODMAP can be powerful, but only if you run it like a structured experiment, not a lifelong sentence.
The Mechanism: What Low FODMAP Is Really Doing
Low FODMAP isn’t a “clean eating” plan. It’s a temporary chemistry experiment on your gut.
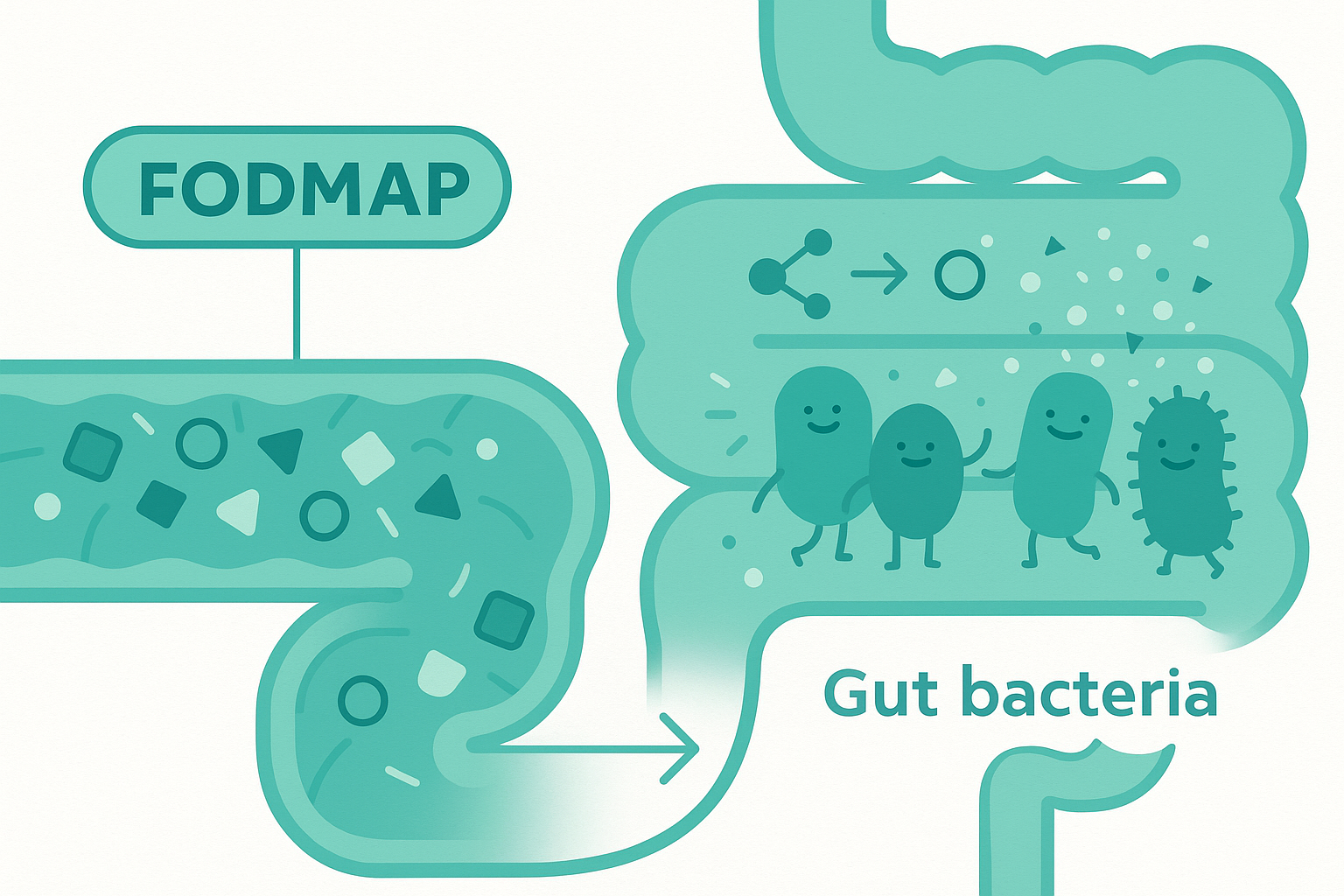
FODMAPs are certain short-chain carbs that your small intestine doesn’t absorb very well. They travel down to your colon, where your gut bacteria throw a fermentation party. That fermentation makes gas. Gas stretches the gut. If you have IBS, your gut nerves are extra sensitive to that stretch. That’s the key problem: not more gas than other people, but more pain and urgency from the same gas.
On top of that, some FODMAPs (like lactose and fructose) pull water into the intestine. Think of them as tiny water magnets. More water + more gas = bloating, cramping, diarrhea, or a weird mix of constipation with upper bloating.
The low FODMAP diet works by reducing the load of these fermentable carbs, so there’s less gas production and less water shift. That means less stretching of the gut wall and fewer “emergency bathroom” moments.
But here’s the important part: it’s not that FODMAPs are “bad.” They’re actually useful fuel for gut bacteria. The problem is the dose and timing in a sensitive system. The diet is meant to identify your personal thresholds, not to wipe FODMAPs from your life forever.
The Clinical Reality: Why Most People Do It Wrong
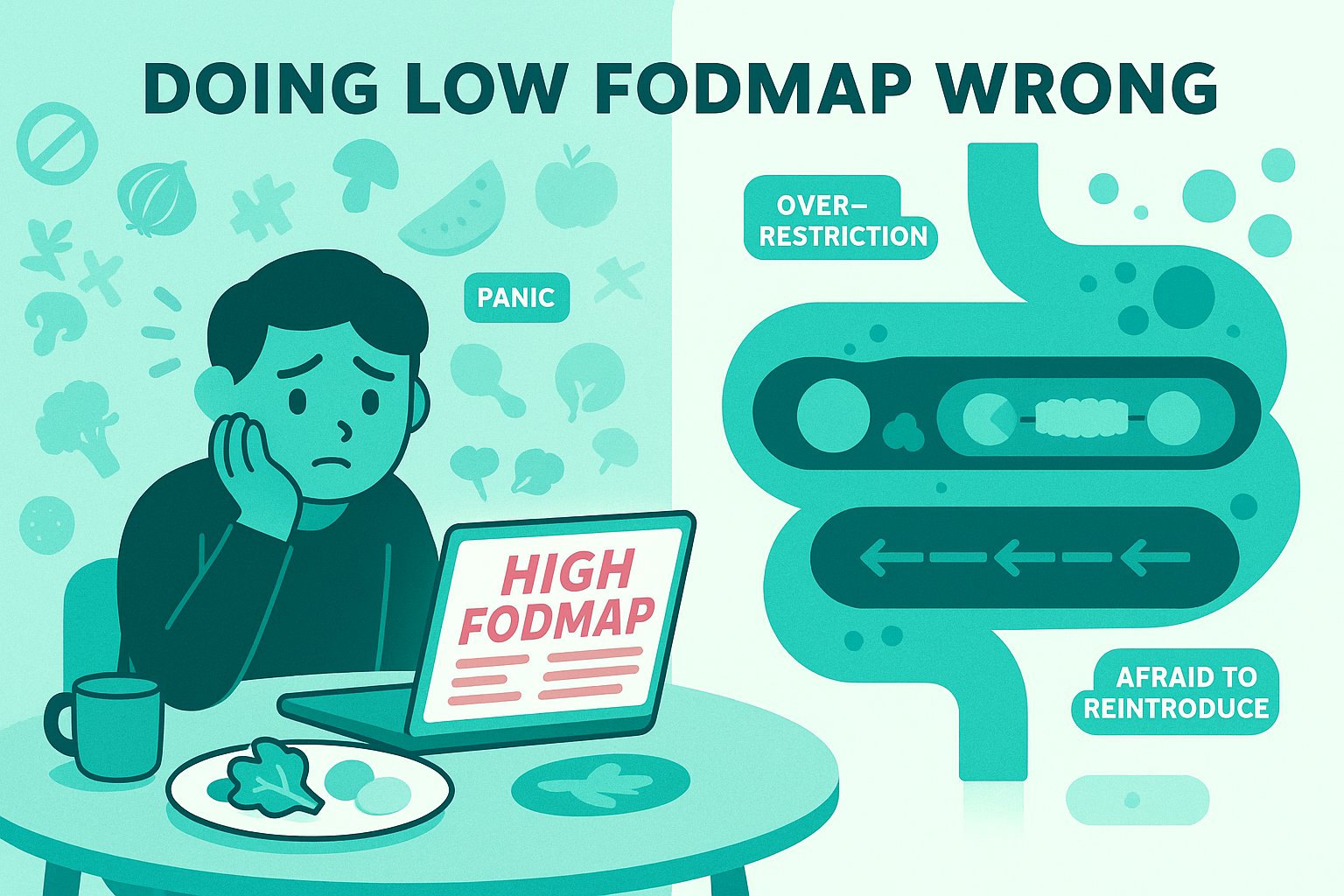
In real life, low FODMAP often looks like this: you Google a list, panic at how many foods are “high,” cut out half your diet overnight, feel a bit better, then plateau, or get stuck, scared to reintroduce anything.
Common patterns I see:
You feel less gassy but more constipated. That’s because you didn’t just cut fermentable carbs, you also accidentally cut a ton of fiber. Less fiber, slower motility, more “brick-like” stools. So yes, your belly is quieter, but now you’re going every 3–4 days and it still hurts.
You feel overwhelmed and underfed. When you try to follow three different FODMAP lists from random blogs, they contradict each other. You end up living on chicken, rice, and maybe blueberries. That’s not a therapeutic plan; that’s a nutritional dead end.
You think it “didn’t work” because symptoms didn’t vanish. The research isn’t “zero symptoms or failure.” It’s meaningful reduction in pain, bloating, and bowel chaos, often 30-70% better. If you’re expecting a perfect gut, you’ll call a solid response a failure.
You stay in elimination mode indefinitely. This is the biggest mistake. The low FODMAP phase is supposed to be short, usually 2–6 weeks. After that, you systematically test foods back in. Staying strict long term can narrow your microbiome and create food anxiety, which is its own IBS trigger.
And then there’s the mental load. Eating out gets stressful. Social stuff feels risky. You start to feel like your gut is a bomb you have to constantly defuse. That stress alone can amplify symptoms, even if your FODMAP game is perfect.
So if you’ve “tried low FODMAP” and it felt like chaos, that’s not on you. It’s a process problem, not a willpower problem.

The Practical Framework: Running Low FODMAP Like a Pro
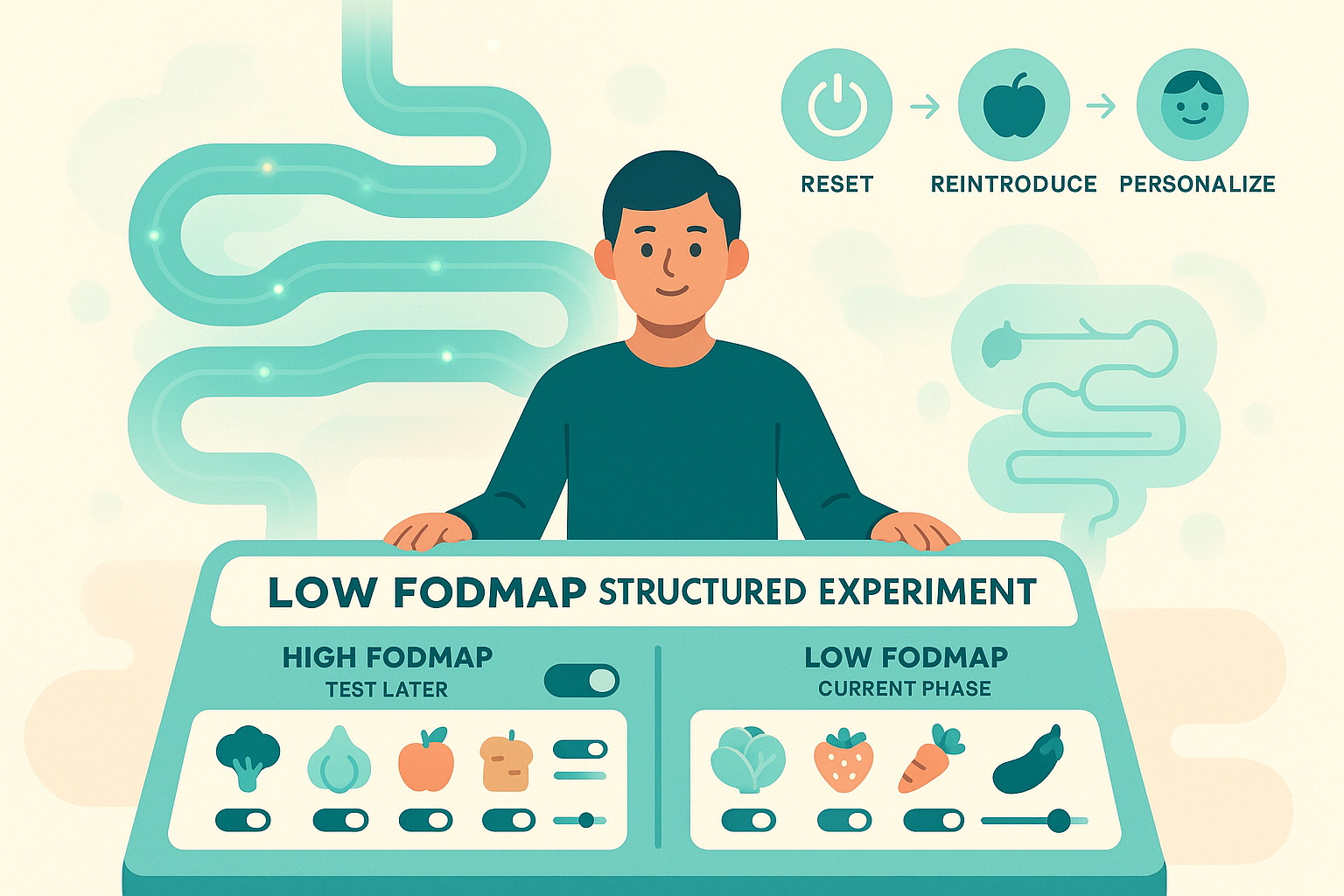
Think of this as a 3-phase project, not a new identity.
Phase 1: Targeted Elimination (2–6 weeks)
This is a controlled reduction, not a purge of joy from your life.
Pick a single, credible source for food lists. The Monash University app is the gold standard—they’re the team that actually developed and tested the low FODMAP diet. Using five different lists just creates confusion.
Your goal in this phase: reduce total FODMAP load, not hit zero. Tiny amounts often don’t matter. A splash of milk in coffee is different from a giant milkshake.
You’re looking for a pattern like: “My average day is less bloated, less painful, and bathroom trips are less dramatic.” Not perfection, just a noticeable shift.
During this phase, don’t forget fiber and balance. Keep some low FODMAP fiber sources in rotation: things like oats, quinoa, kiwifruit (in low FODMAP portions), carrots, zucchini, firm tofu. That helps avoid the “I fixed my gas but broke my bowels” problem.
And track. Not obsessively, but enough to see patterns. A simple note in your phone: what you ate, symptom timing, stool form (using a simple 1–7 scale like the Bristol chart). You’re collecting data, not judging yourself.
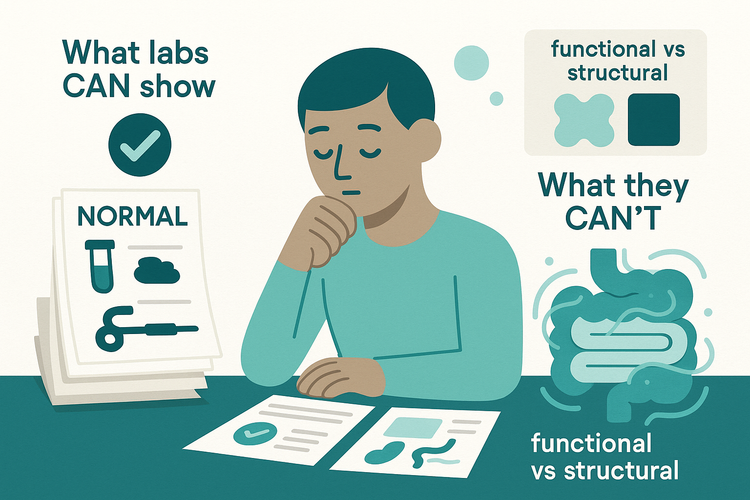
If after 3–4 weeks your symptoms are exactly the same, fully strict low FODMAP may not be your lever, or there are other dominant drivers (motility issues, pelvic floor, bile acid diarrhea, etc.). That’s useful information too.
Phase 2: Structured Reintroduction (6–8+ weeks)
This is where most people skip—and where the real value lives.
Each FODMAP group gets tested separately: lactose, excess fructose, fructans (like wheat/garlic/onion), galacto-oligosaccharides (GOS, in beans/legumes), and polyols (sorbitol, mannitol).
You pick one group, one test food, and one week. For example: wheat bread for fructans.
Day 1: small portion. Day 2: medium portion. Day 3: large portion. Then 3–4 days back to baseline low FODMAP, watching symptoms.
You’re not looking for “I felt something” after every test. You’re looking for reproducible, meaningful flares: bloating within a few hours, pain, urgency, or clear stool changes tied to higher doses.
If you react strongly at a low dose, that FODMAP group is a big trigger. If you only react at high doses, your tolerance is decent, you just need to watch portion stacking. If you don’t react at all, that group is probably safe to bring back.
Run through each group like this. Yes, it takes time. But at the end, you have a personal map instead of living by someone else’s fear list.
Phase 3: Personalization and Liberalization (long term)
Now you build your “IBS-friendly, not IBS-perfect” way of eating.
Let’s say your testing showed:
Lactose: small amounts okay, big glasses of milk = disaster. Fructans: onion and garlic are bullies; wheat in small amounts is fine. Polyols: no obvious issues
That means you don’t need to avoid all dairy forever. You might use lactose-free milk for big servings but enjoy regular yogurt or cheese. You might cook with garlic-infused oil instead of whole garlic but still have a slice of sourdough without panic.
You also watch FODMAP stacking. Maybe you’re fine with a small serve of chickpeas, or a slice of wheat bread, or a bit of apple, but not all three in one meal. That’s load, not “good vs bad” food.
And you keep an eye on context. Sleep, hormones, stress, infections, travel, all change your gut’s sensitivity. A food that’s fine most weeks might bother you during a flare. That doesn’t mean it suddenly became “toxic.” It just means your threshold moved.
Two more pro-level points:
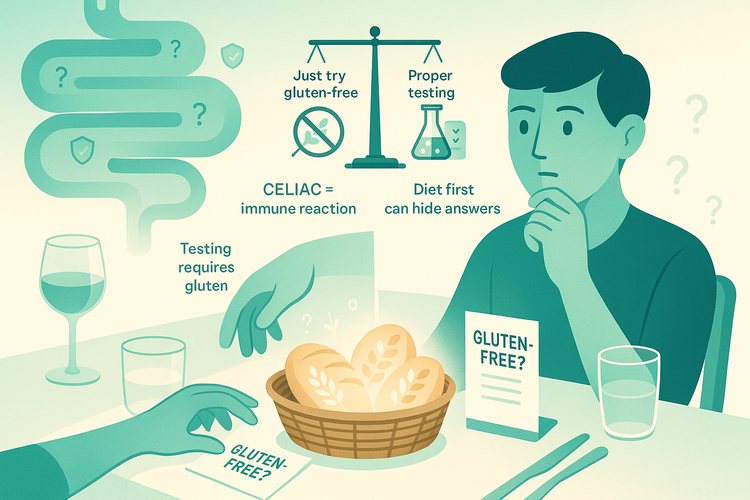
First, low FODMAP is evidence-based for IBS, especially IBS-D and mixed types. It’s not a cure for every digestive issue. If you have red-flag symptoms (weight loss, blood in stool, waking from sleep with pain or diarrhea, anemia), this is not your starting point. You need proper workup.
Second, supplements, random food intolerance tests, and influencer protocols don’t replace this structured approach. Most “food sensitivity panels” are measuring antibodies that reflect exposure, not damage. They create huge avoid lists with very little science behind them. Low FODMAP, when done correctly, is about testing your actual lived response, not lab noise.
Closing: Use the Diet, Don’t Let It Use You
Low FODMAP, done well, is a temporary, targeted investigation, not a personality trait and not a lifelong prison. You strip things back just enough to calm the chaos, then you methodically challenge your system to find your real limits.
The goal isn’t a perfect gut. It’s a gut you understand well enough that food feels like a set of levers, not landmines. In the next article, we’ll dig into what to do when low FODMAP helps “a bit” but not enough, because diet is only one piece of the IBS puzzle.