Endoscopy 101 - Your Guide to EGD and Colonoscopy | Gut Check Daily Explains

Endoscopy 101 Your Guide To Egd And Colonoscopy
Download this comprehensive checklist to bring to your next GI appointment. Get evidence-based answers and a clear action plan.
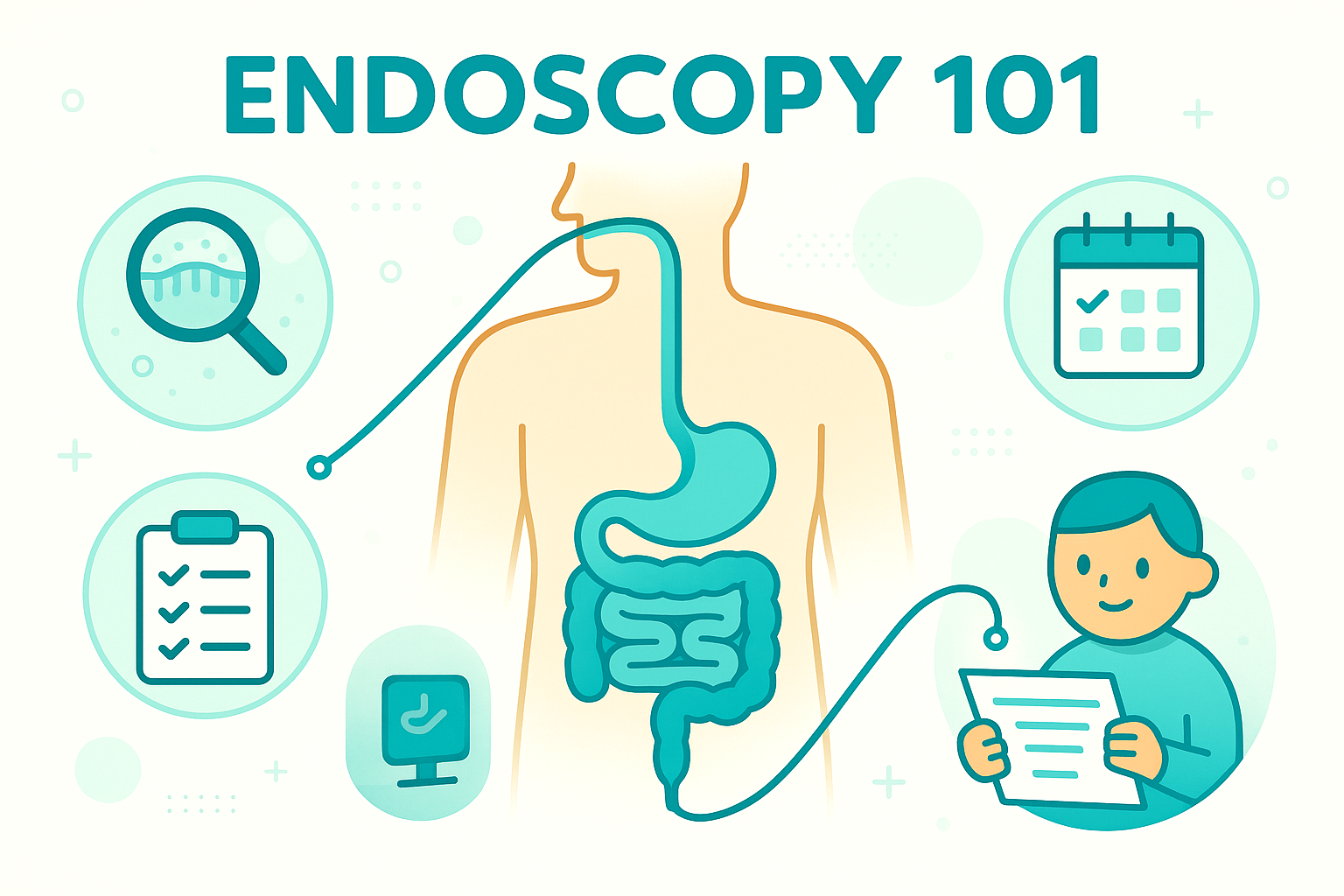
📥 Download PDF Checklist →Stool tests, breath tests, blood tests all have a place. But when we actually need to see what’s going on in your gut, we’re back to the old, unglamorous workhorse: endoscopy. Let’s walk through what that really means, without the horror-movie version your brain is playing.
The Mechanism: What an Endoscopy Actually Does
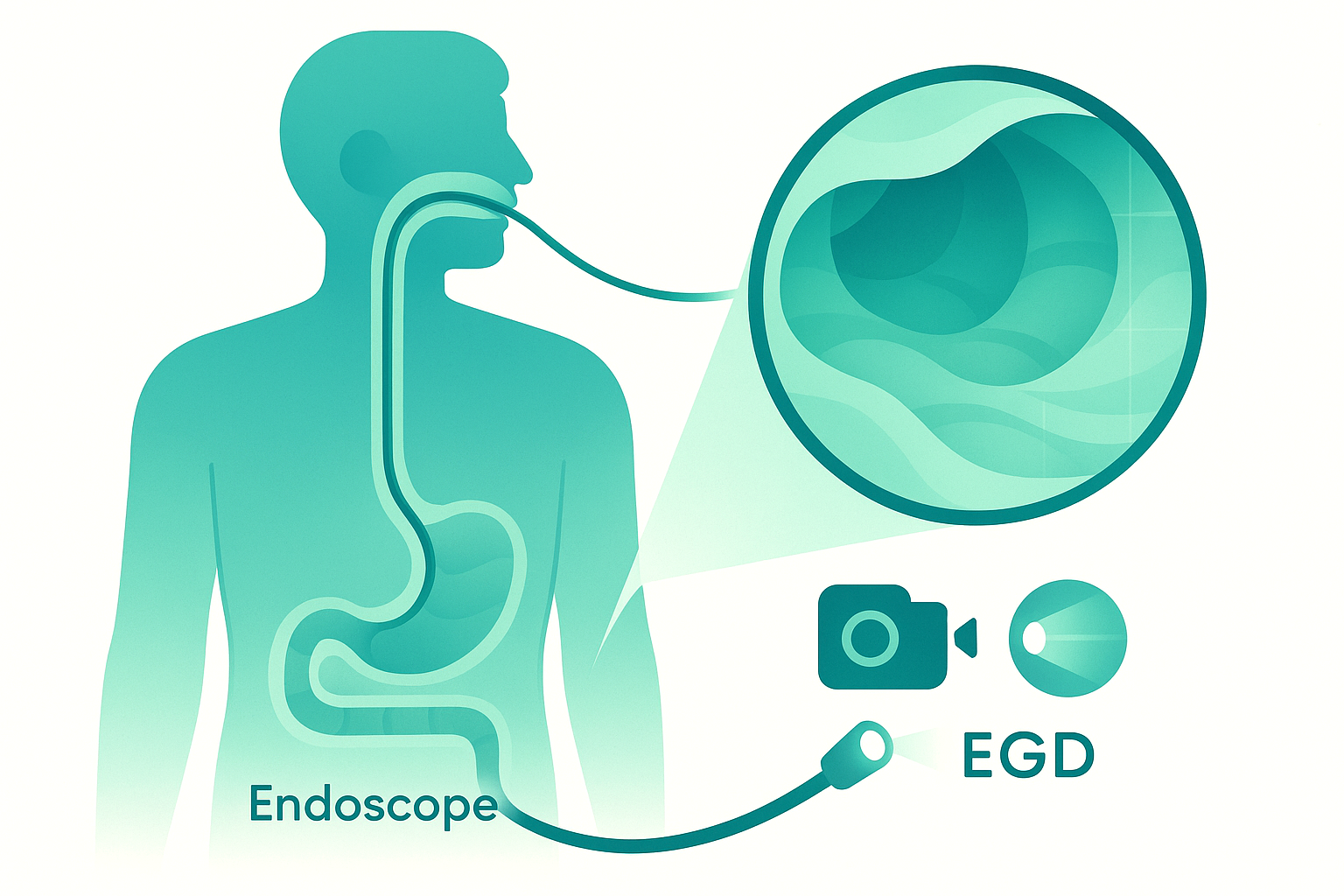
Endoscopy is just a camera on a flexible tube. That’s it. No lasers. No scraping your insides raw. No “cleaning you out” in some vague detox way.
There are two main versions for the digestive tract:
An EGD (esophagogastroduodenoscopy) goes from your mouth down your esophagus, through your stomach, into the first part of your small intestine. Think of it as checking the entry corridor and lobby of the gut.
A colonoscopy goes in from the other end and looks at the colon and the very end of the small intestine. That’s the exit hallway and loading dock.
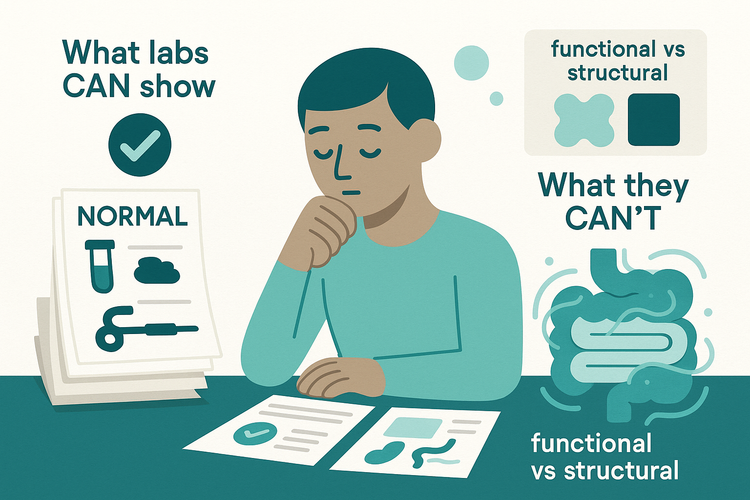
Here’s why this matters: most other tests are indirect. Blood work, stool tests, imaging, they’re all guessing what’s happening based on clues. Endoscopy is direct evidence. We see inflammation instead of just guessing from markers. We see polyps instead of waiting for blood in the stool. We see ulcers, celiac-type damage, strictures, angiodysplasia, microscopic colitis, and more.
And it’s not just looking. We can biopsy (tiny tissue samples), remove polyps (small growths), stop bleeding, stretch narrowed areas, and treat some lesions right then and there. The scope is basically a camera with a Swiss Army knife attached.
Sedation means you’re comfortable and usually remember very little. Your brain imagines something far more brutal than what actually happens. Physiologically, this is a controlled, low-trauma procedure with a very low complication rate when done properly.
The Clinical Reality: How This Shows Up in Real Life
Here’s how this plays out in the real world.
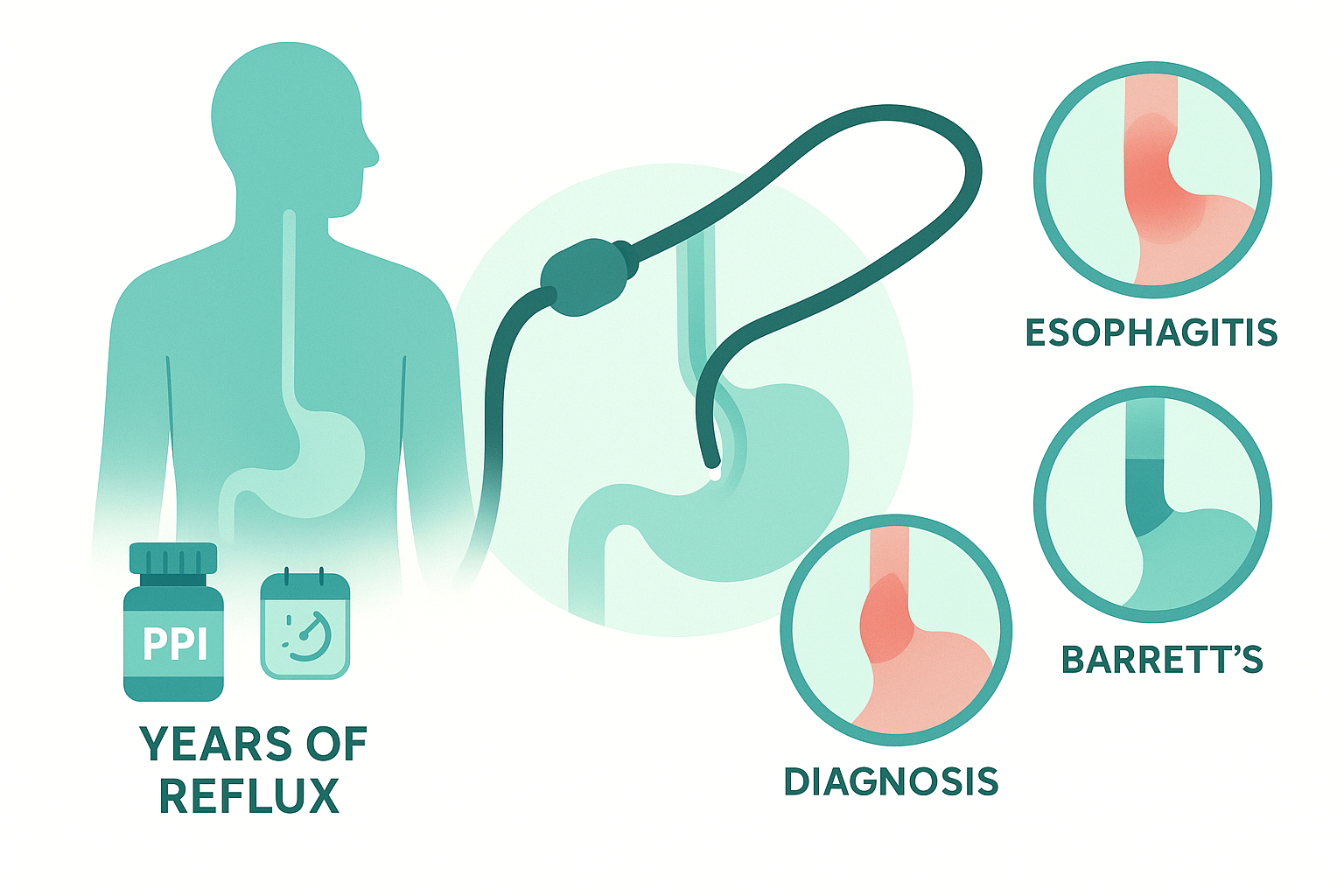
You’ve had reflux for years. PPIs help, but not fully. Someone finally orders an EGD. We look, and instead of guessing, we see whether your esophagus is inflamed, whether there’s Barrett’s tissue (precancerous change), whether there’s a hiatal hernia, or whether your symptoms are from something else entirely, like eosinophilic esophagitis. Same symptom label, very different underlying problems.
Or you’re 47 and your primary care doc brings up colonoscopy. You feel fine. No blood, no pain, no weight loss. This isn’t because we expect to find cancer in everyone; it’s because colon polyps are quiet for years. They sit there, growing, not causing symptoms, until they eventually can turn into cancer. Colonoscopy is one of the rare tests in medicine that’s both diagnostic and preventive. We find polyps, we remove them, we lower your future cancer risk. That’s not wellness marketing, that’s decades of data.
On the flip side, some people get scoped too late. They’ve had “IBS” for years, then one day someone finally checks, and it’s actually inflammatory bowel disease, microscopic colitis, or celiac disease. Those aren’t things you pick up reliably from a breath test or a TikTok elimination diet.
Conventional advice often fails because it treats symptoms in isolation: “You’re bloated? Try low FODMAP.” “You’re tired? Take iron.” Without asking, “Do we actually know what your gut lining looks like?” Endoscopy isn’t the answer for everyone, but when it’s indicated and delayed, people can spin in circles for years.
And yes, the prep and the idea of a camera inside you is not fun. The fear is real. But the alternative, flying blind while your gut quietly smolders, isn’t great either.
Practical Framework: When, Why, and How to Think About Scopes
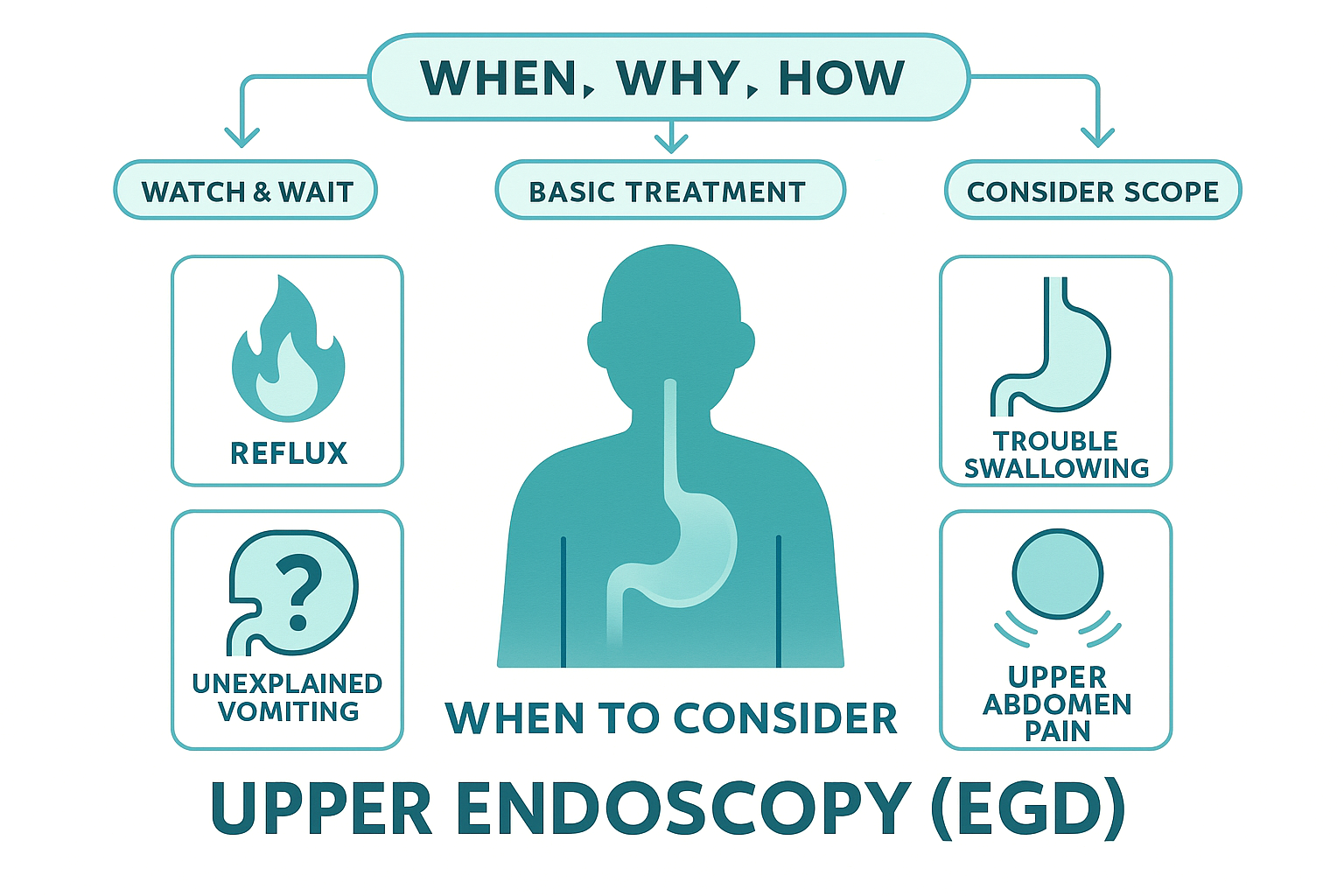
Let’s strip this down to a decision framework you can actually use in your own head.
1. What problem are we trying to solve?
EGD is usually considered when you have things like persistent reflux, trouble swallowing, unexplained vomiting, upper abdominal pain that isn’t responding to basic treatment, anemia without a clear cause, or suspected celiac disease.
Colonoscopy comes into play for colon cancer screening, unexplained changes in bowel habits, rectal bleeding, unexplained iron deficiency, chronic diarrhea, or to monitor known conditions like IBD or polyps.
If your doctor is suggesting a scope and you’re hesitant, ask directly: “What specific question are you hoping this endoscopy will answer or rule out?” If they can’t answer that clearly, push for clarity.
2. What can this test do that others can’t?
If the answer is “we’ve tried noninvasive tests and still don’t know what’s wrong,” or “we need to rule out structural problems or precancerous changes,” then endoscopy makes sense.
Stool tests can’t show you if your esophagus is narrowing. Anemia panels can’t see a colon polyp. CT scans can miss flat lesions or subtle inflammation. There’s a reason endoscopy hasn’t been replaced by some fancy new blood test: seeing tissue directly is still the gold standard for many conditions.
3. Understand the real risks and benefits.
Complications like perforation and major bleeding are rare, especially in routine diagnostic scopes and in experienced hands. Sedation is generally safe, though not zero risk. The benefit side is big: catching cancer early, preventing cancer by removing polyps, diagnosing conditions that actually change your treatment plan.
If your risk is higher, such as if you have severe heart or lung disease, are on blood thinners, or have prior surgical anatomy, your GI doc should walk you through how they’re minimizing that risk.
4. Prep and recovery: what it actually feels like.
For colonoscopy, the prep is the worst part, no question. It’s not “destroying your microbiome” or “stripping your gut lining.” It’s flushing stool out so we can see the wall of the colon. Your microbiome bounces back; you’re not erasing it.
You’ll spend a night making friends with your bathroom. Then you go in, get an IV, drift off with sedation, and wake up groggy with some gas. There's often a lot of waiting around, but most people say, “That was it?” EGD is even simpler: no bowel prep, just fasting, sedation, scope, done.
5. Use it as a data-gathering moment, not just a hurdle.
Ask for a copy of your report and pathology. Learn the words: polyp type, inflammation pattern, biopsies taken where. This isn’t about turning you into a mini-GI, but about you actually owning your health data instead of vaguely remembering “it was normal… I think?”
Endoscopy is not a wellness ritual. It’s a targeted tool. The power comes from using it at the right time, for the right reasons, and then actually acting on what it shows.
Endoscopy, EGD and colonoscopy, isn’t about being “extra cautious” or “doing all the tests.” It’s about choosing the one test that lets us stop guessing and actually look. When you understand what it’s for, what it can and can’t do, and how it fits into your bigger gut story, it stops being a monster under the bed and becomes what it really is: a camera, a few biopsies, and a chance to catch problems before they catch you.
Next time, we’ll get into what those biopsy terms actually mean, so “mild chronic inflammation” on your report doesn’t just sit there haunting your patient portal.