Celiac Disease Diagnosis: Why just try gluten free misses the point
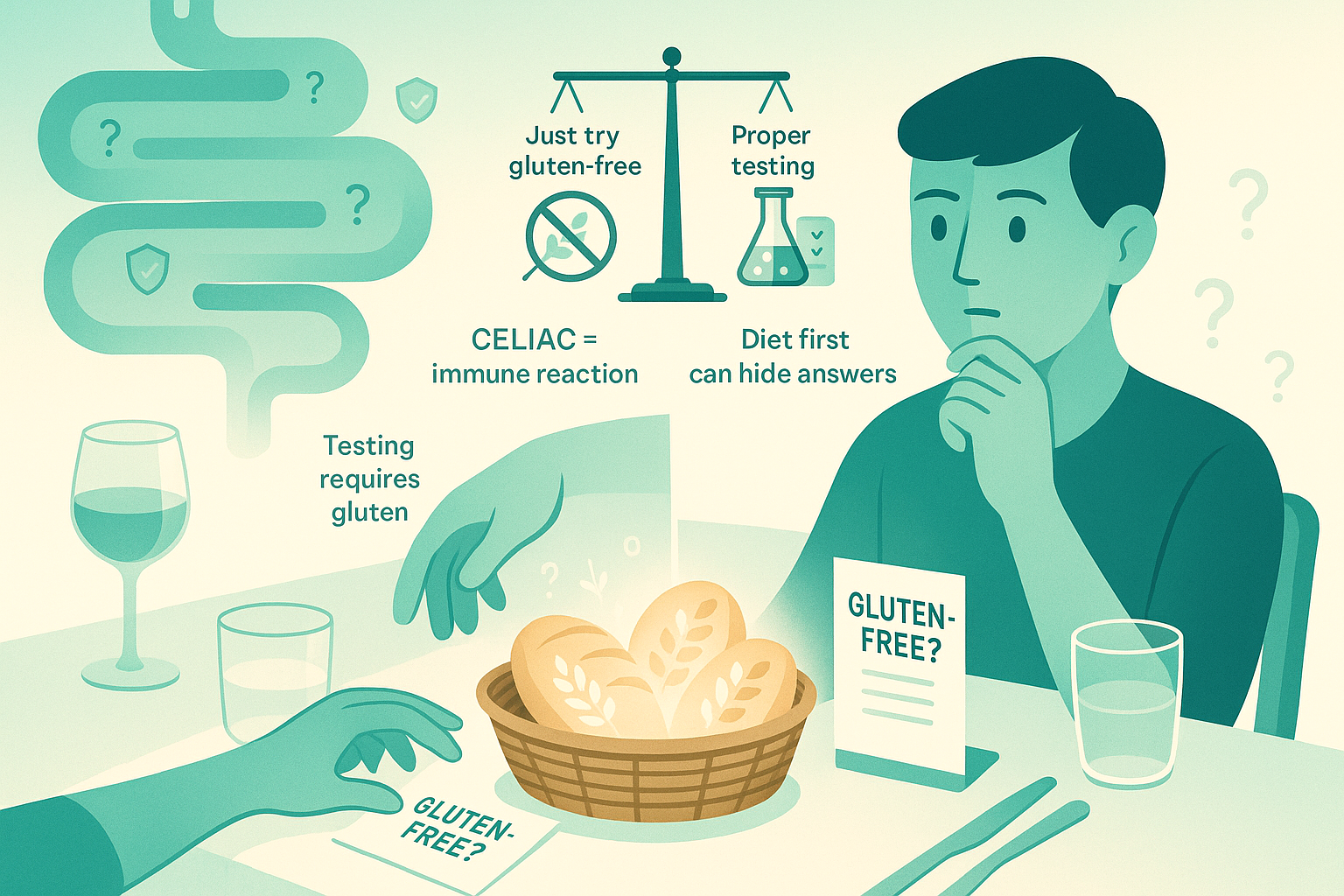
You’re 10 minutes into a date, the bread basket just hit the table, and your brain goes into debate mode: “My stomach’s a mess… maybe I should just try gluten-free and see what happens.” Your friend with “IBS” swears it changed their life. Instagram agrees. The problem? For celiac disease, “just try gluten-free” can actually block you from getting a real diagnosis when it matters most.
Let’s unpack why that shortcut backfires.
The Mechanism: What Celiac Actually Is (and Isn’t)
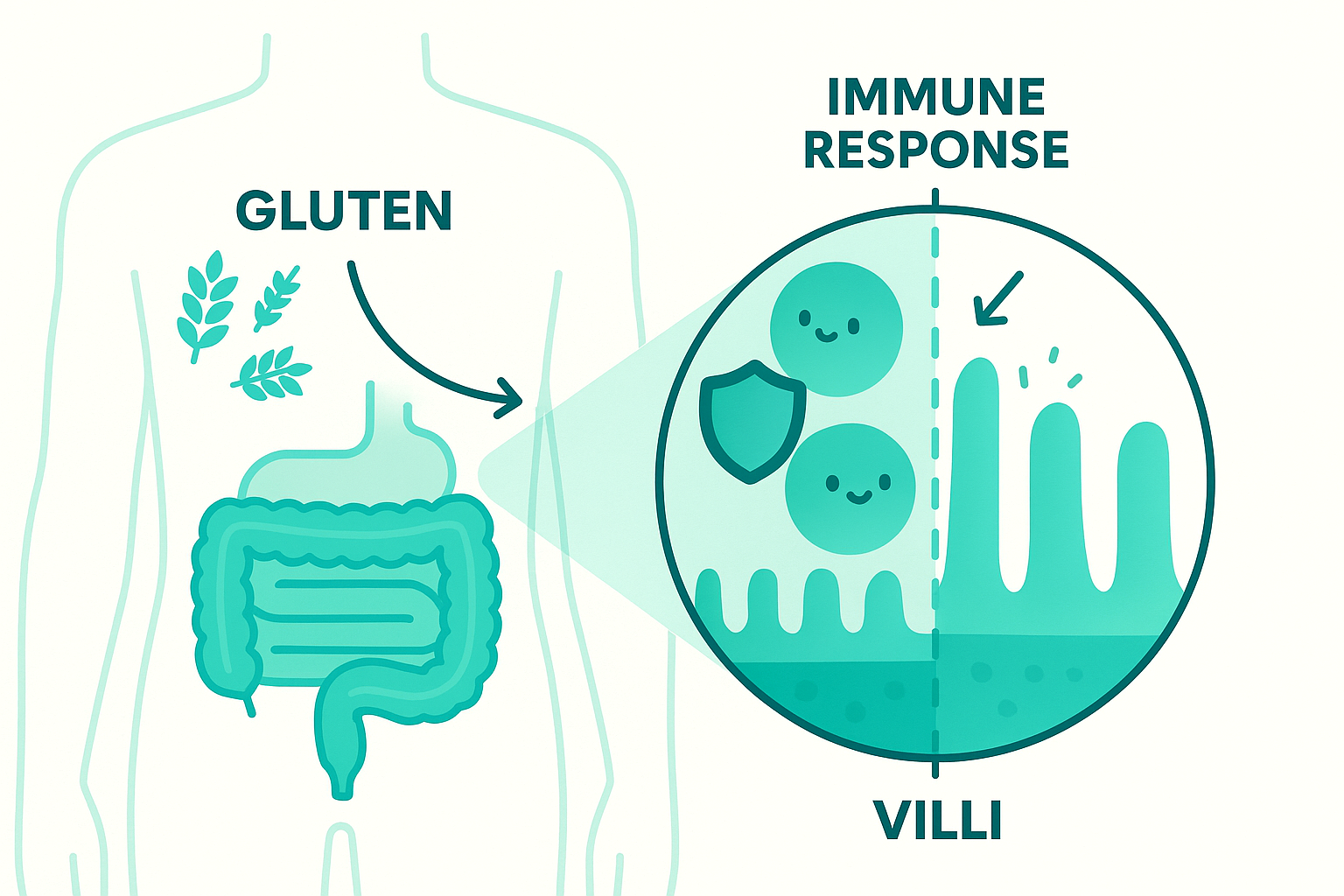
Celiac disease is not a “gluten sensitivity.” It’s an autoimmune disease.
Your immune system is supposed to fight infections. In celiac, when gluten shows up (from wheat, barley, rye), your immune system attacks your own small intestine, specifically the villi: those tiny finger-like projections that absorb nutrients.
Think of your small intestine as a shag carpet. All that surface area is how you pull in iron, B12, calcium, protein, fats, and more. In untreated celiac, the immune attack slowly turns that shag carpet into a worn-down doormat. Less surface area. Less absorption. More problems.
This isn’t just about gas and bloating. It’s about:
Iron deficiency anemia that doesn’t fully respond to supplements, Low bone density or fractures, Fertility issues, Unexplained weight loss (or sometimes weight gain with malabsorption), and Neurologic symptoms, mouth ulcers, fatigue.
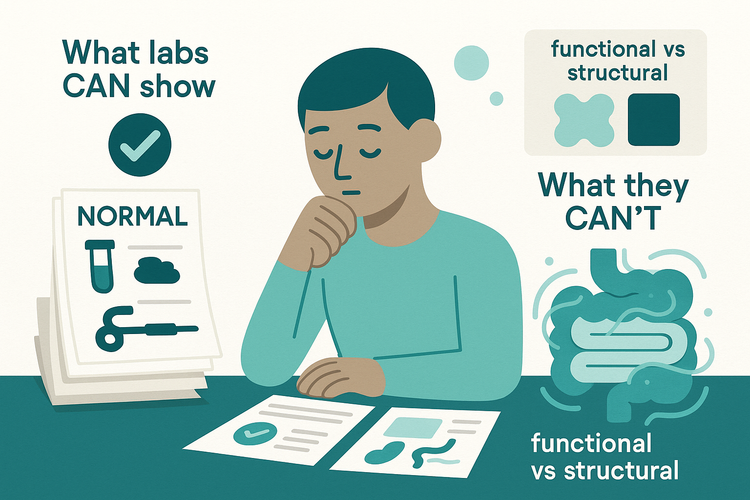
Here’s the key: that immune reaction leaves detectable fingerprints in your blood and in your intestinal tissue. We can see specific antibodies. We can see damage under the microscope on a biopsy.
But only if gluten is still in your system.
Once you pull gluten out, the immune attack calms down. Antibodies fall. The shag carpet starts growing back. That sounds great, except it also makes your tests look “normal,” even if you do have celiac.
That’s why “just try gluten-free” before testing is such a trap.

Clinical Reality: How “Just Try Gluten-Free” Derails Diagnosis
Here’s how this usually plays out in real life.
You’ve had bloating, diarrhea, or constipation for months or years. Maybe you’re tired all the time. Maybe your iron is low. You Google. You see “gluten” in every headline. A friend says, “Just cut it out and see.”
So you do. And maybe you feel a bit better. Or a lot better. Now you’re thinking: “So I must have celiac, right?”
Not necessarily.
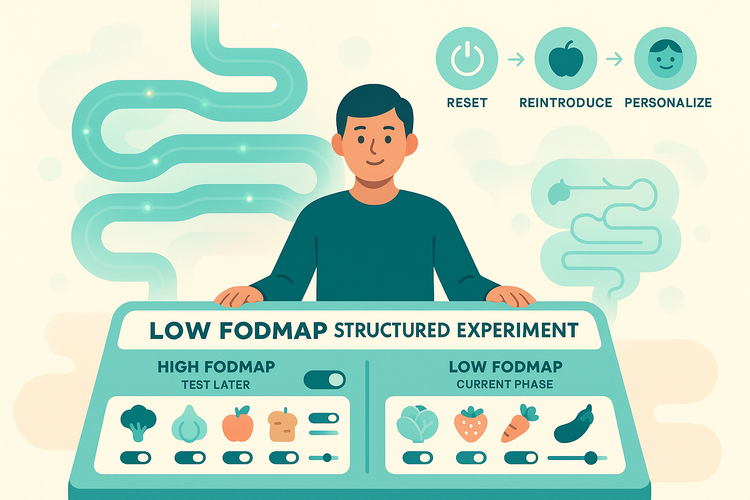
Some people have non-celiac gluten sensitivity. Some react more to FODMAPs (fermentable carbs in wheat) than to gluten itself. Some have IBS and feel better because they cut out a bunch of ultra-processed foods along with gluten. The internet rarely explains these differences.
Now fast forward. Months or years gluten-free. You finally see a doctor and say, “I think I have celiac.” We run the standard blood tests (tTG-IgA, total IgA, maybe others). They come back normal. Why? Because your immune system isn’t currently being triggered by gluten.
To get accurate testing, you’d need a gluten challenge: eating a meaningful amount of gluten daily, usually for weeks, sometimes longer, before blood tests and endoscopy. For someone who feels awful with gluten, that’s a hard sell.
So you end up in limbo: No clear diagnosis, No baseline bone density, vitamin levels, or other screening, No formal follow-up plan, A “gluten-free” life without knowing how strict you truly need to be.
And here’s the kicker: true celiac requires lifelong, strict gluten avoidance. Not “I pick off the croutons” strict. We’re talking label reading, cross-contamination awareness, and medical follow-up over time. That level of commitment should be based on actual evidence, not vibes.
Skipping proper testing makes everything fuzzier, for you and for your doctors.
Practical Framework: How to Do This the Smart Way
If you’re wondering about celiac, the most important rule is simple:
Don’t go fully gluten-free before proper testing.
If you’re still eating gluten now, this is the window where tests are most accurate.
Here’s a practical way to think about it.
First, ask yourself: Am I currently eating gluten most days? If yes, and you have symptoms like chronic GI issues, iron deficiency, low B12, weight changes, fatigue, family history of celiac, thyroid disease, type 1 diabetes, or unexplained bone loss—this is the time to talk to your doctor about celiac blood tests before experimenting with diet.
Those tests usually include tTG-IgA and total IgA, sometimes others. If they’re positive, the next step is often an upper endoscopy with small bowel biopsies while you’re still on gluten. That’s how you get a clear, evidence-based diagnosis.
If you’ve already gone gluten-free, don’t panic. You have options, but they’re more complicated.
You and your doctor can discuss: Whether your history strongly suggests celiac, Whether a gluten challenge is worth it for you (how much gluten, how long, what symptoms to expect), Whether there are other explanations for your symptoms that should be checked regardless.
Some people choose to stay gluten-free without a formal diagnosis. That’s your choice, but go into it with eyes open:
Without a confirmed diagnosis, people tend to be less strict over time. That’s fine if the issue is non-celiac sensitivity. It’s not fine if you actually have celiac, where “cheating” isn’t just about symptoms, it’s about long-term risks like osteoporosis and, in a small subset, intestinal lymphoma.
So the framework is:
Use symptoms as a signal, not a diagnosis. Use testing while you’re still eating gluten to get clarity. Use diet changes after proper evaluation, not instead of it.
Closing: The Point Isn’t Just the Bread
“Just try gluten-free” sounds simple and harmless. For celiac disease, it’s like painting over a crack in the foundation before anyone inspects the house. You might feel better for a while, but you’ve lost the chance to really understand what’s going on underneath.
If gluten is on your suspect list, the goal isn’t to rush into restriction. It’s to get the right information, at the right time, so you can make decisions that protect both your gut and your long-term health. In the next piece, we’ll dig into what a smart gluten challenge actually looks like, and who truly needs one.